Improved tolerance of radical lung surgery after contralateral diaphragmatic elevation correction in lung cancer patients: a stepwise approach
Introduction
Surgery is the best treatment option in early stage lung cancer. Limited pulmonary function is a contraindication to surgery and can be overcome in some cases with smoking cessation, anti-obstructive medication and pulmonary rehabilitation. Contralateral phrenic nerve palsy is a rare cause of functional impairment. To give the patient the best chance of survival with curative resection, a contralateral diaphragmatic plication can be the first step to increase lung volumes and allow sequential tumor resection on the opposite lung.
Case presentation
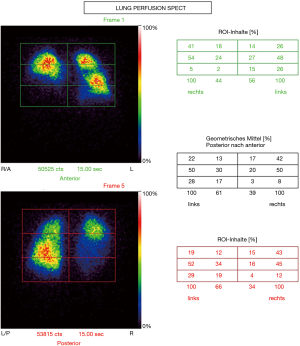
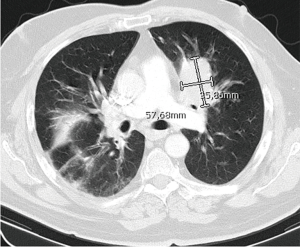
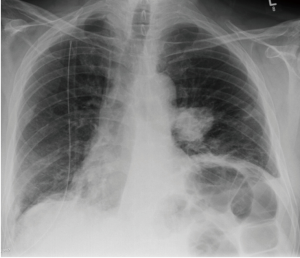
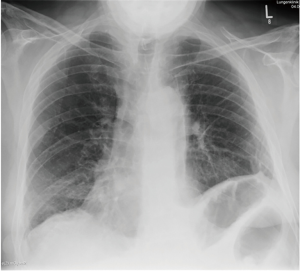
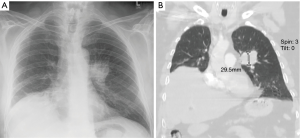
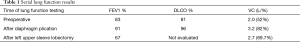
A 69 years old ex-smoker with 30 pack years was admitted in our tertiary lung cancer center with a 5cm left upper lobe mass. Before admission into our center, he was first treated for left sided pneumonia in a neighbouring clinic. He was suffering from diabetes, hypertension and a severe endogenous depression with panic attacks causing breathlessness in various situations. With a body mass index of 35, and ECOG score of 2, the patient was on Amitriptylin 60 mg bd, Loracepam 0.5 mg, Risperidon 3 mg bd, beside Insulin and multidrug antihypertensive treatment. He had a FEV1 83%, DLCO 81%, TLC 5.6L (84%) and a 39% perfusion of the right lung (Figure 1). After Bone scan, MRI brain and a rigid bronchoscopy with endobronchial ultrasound and transbronchial needle aspiration, we arrived at a final diagnosis of squamous cell cancer (G3) of the left upper lobe (cT3, cN1, cM0) (Figures 2,3). Expecting a severe post-operative functional deterioration, the patient refused surgery. Since the tumor bearing (left upper) lobe still had relevant ventilation and perfusion, a lobectomy would have resulted in severe pulmonary functional decline. After comprehensive discussion in our interdisciplinary tumor board, a diaphragmatic plication was recommended to overcome postoperative respiratory distress. The patient with an ECOG score of 2, multiple psychiatric conditions and a lack of compliance was not seen as an optimal candidate for multimodality therapy, but was in agreement to sequential operative interventions. A right sided open diaphragm plication with covering of the whole diaphragm with a non-absorbable polypropylene mesh (Bard®, Warwick, USA) was performed, without any post-operative complications (Figure 4). After 4 weeks of recovery he was re-admitted and re-evaluated. His lung functions had improved to FEV1 91% and DLCO 96% (Table 1). So a left upper sleeve lobectomy with radical lymphadenectomy and pericardial fat pad application was performed. Pathologic specimen work-up revealed a squamous cell carcinoma pT3 N0 (0/19) L0 V0 G2 R0, UICC stage II B. The further course was uneventful and he was discharged on the 10th postoperative day (Figure 5). Adjuvant chemotherapy was not administered because of bad patient compliance. Although the spirometry during the 8th postoperative week showed a deterioration of his FEV1 (66.6%) and vital capacity (69%) and a non-measurable DLCO due to patient noncompliance during the examination (Table 1), the clinical state of the patient showed no significant reduction in the lung functions.
Full table
Discussion
Since 1920, diaphragm plication has been performed for various indications. Tokunaga et al. 2010 demonstrated the efficacy of intra-operative unilateral diaphragm plication in patients undergoing unilateral phrenectomy during extended surgery. Patients with diaphragm plication had no additional loss of lung function more than preoperative predicted values and there was no increase in the post-operative complications (1,2). A 10% improvement in FEV1 and vital capacity and a 13% increase in tidal volume in a case series with 9 patients was reported after diaphragm plication for phrenic nerve palsy (3).
Although the first lung function results concerning the reported case theoretically allowed primary resection, the physical performance (ECOG 2, right sided phrenic nerve palsy, right sided reduced perfusion, the high percentage of left upper lobe perfusion) and the subjective shortness of breath lead us to categorize the patient as a high risk candidate. In order to still allow radical cancer surgery as well as a good functional outcome with minimal risk for complications we suggested this sophisticated stepwise approach. This concept of contralateral diaphragm plication to improve pulmonary function prior to limit cancer resection was described by other authors before (4).
Conclusions
Contralateral diaphragm plication prior to radical lung cancer surgery is an innovative and rational stepwise option to treat otherwise inoperable patients.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/ccts.2019.08.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tokunaga T, Sawabata N, Kadota Y, et al. Efficacy of intra-operative unilateral diaphragm plication for patients undergoing unilateral phrenectomy during extended surgery. Eur J Cardiothorac Surg 2010;38:600-3. [Crossref] [PubMed]
- Takahashi Y, Miyajima M, Mishina T, et al. Thoracoscopic one-stage lobectomy and diaphragmatic plication for T3 lung cancer. J Cardiothorac Surg 2018;13:86. [Crossref] [PubMed]
- Welvaart WN, Jak PM, van de Veerdonk MC, et al. Effects of diaphragm plication on pulmonary function and cardiopulmonary exercise parameters. Eur J Cardiothorac Surg 2013;44:643-7. [Crossref] [PubMed]
- Matsui Y, Yoshida S, Iwata T, et al. A strategy for pulmonary resection after contralateral diaphragm plication: a surgical case report. Surg Case Rep 2019;5:88. [Crossref] [PubMed]
Cite this article as: Abdelrahim M, Gupta V, Welter S. Improved tolerance of radical lung surgery after contralateral diaphragmatic elevation correction in lung cancer patients: a stepwise approach. Curr Chall Thorac Surg 2019;1:8.