
在高难度病例中进行胸腔镜肺叶切除术用于肺癌的治疗:技术方面研究
引言
几年来,美国国家综合癌症网络(NCCN)非小细胞肺癌(NSCLC)实践指南推荐使用电视辅助胸腔镜手术(VATS),仍然要遵守肿瘤学治疗标准和解剖原则[1]。一些报告显示,VATS肺叶切除术对于可切除NSCLC是安全的,与传统开胸手术相比,VATS手术能够缩短住院时长,更快恢复正常活动,并展现出术后生活质量更高的优点[2,3]。在具备专业微创胸部外科的大型医疗中心中,随着经验的积累以及仪器和视频技术的更新,使得VATS手术对复杂病例的治疗成为了可能。特别是胸膜腔广泛粘连、叶裂发育不全、术前放化疗、既往胸部手术史、胸壁侵犯、中央型肺癌这些曾被视为VATS手术的相对禁忌的情况,都可以通过VATS手术得到很好的治疗[4,5]。
NSCLC中的T分期
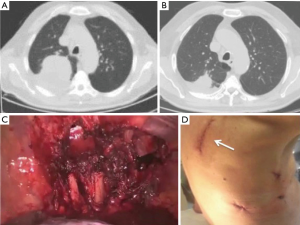
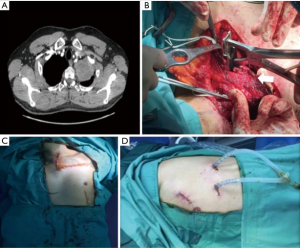
经过仔细的淋巴结和全身评估分期后,对于胸壁受侵的非小细胞肺癌患者可在内镜肋骨切割器械的协助下完成VATS手术。在本文选定病例中,也可以使用传统肋骨切割器通过小切口完成对受侵肋骨的切除,同时联合VATS手术完成对肺部肿瘤的切除。此方法无需扩张肋骨和肩胛骨(图1)。然而,当存在以下的情况时不适用以上方法,包括需要切除4根或4根以上肋骨,横突受累或胸壁受侵范围过大,手术不足以满足切除范围[6]。我们的经验表明,即使是在肺上沟癌侵犯第一肋骨的NSCLC患者中,这种混合入路的方法也同样有用:1997年有过相关研究,在这种情况下,可以通过锁骨、胸锁乳突肌、第一肋骨和胸骨形成的肌骨瓣来填补术区,能够使胸腔镜肺叶切除术联合传统胸壁切口进行胸壁部分切除这类的手术得以完成[7](图2)。随着微创手术经验的增加,即使是肿瘤的大小也成为了VATS肺叶切除术的相对禁忌症:由于新辅助化疗后通常会出现胸膜增厚、胸膜腔粘连加重、毛细血管增多的现象,这都有可能导致无法识别正确的解剖结构。通过仔细肺门分离和减小肺部牵拉,都可以很好地避免由于小血管破裂造成的出血。当中心型肺癌靠近大血管的患者行全肺切除又无法避免并发症的发生时,这种先进的电视胸腔镜技术尤为适用,并特别推荐行“袖式切除”[8]。此外,对于存在既往肺部手术史的患者,即使是早期的非小细胞肺癌仍要需要较高的VATS手术操作技巧。这是由于这部分患者存在肺门周围纤维化、广泛的胸膜腔粘连。在这种情况下,肺部的血管分离可能存在难度,当其与心包紧密粘连的时候,可能还需要切除部分心包[9]。此外,当胸膜腔紧密粘连,仅存在狭窄的缝隙情况下,为避免VATS术后肺部漏气,我们建议采用所谓的隧道技术[10]:这种技术的使用可以完成叶间淋巴结的评估并能充分暴露支气管、血管(图3)。对于既往通过正中胸骨切开术使用左乳内动脉(LIMA)或右乳内动脉(RIMA)进行“冠脉搭桥术”的患者,因为胸膜粘连的广泛存在,即使是早期的非小细胞肺癌,治疗起来也是具有相当大的挑战。分离胸膜腔粘连时必须谨慎注意避免损伤LIMA或RIMA移植物。
NSCLC中的N1组淋巴结
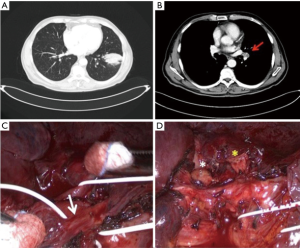
系统性淋巴结清扫术是NSCLC手术治疗的标准术式,可进行充分的病理分期。然而,当肺门淋巴结存在转移融合时,此类手术治疗可能很复杂:这种情况通常需要切开血管鞘并分离鞘内的血管,同时由于巨大的淋巴结掩盖了局部解剖结构,因此在分离时操作应更加细致,联合锐性和钝性分离,以避免对异常动脉或静脉分支的意外损伤[11]。与支气管、血管融合紧密粘连的肺门淋巴结转移病例,使得微创手术操作更加困难,这可能导致动脉损伤引起的术中出血。这种情况是VATS肺叶切除术中转开胸的主要原因之一[12]。相对于微创外科经验较低的医生而言,经验丰富的VATS外科医生可能会更好的处理淋巴结侵犯血管、支气管的情况,进而完成肺动脉、支气管袖式切除术[13,14]。在本文选定的左肺下叶肺癌伴叶间淋巴结转移、囊外侵犯的病例中,正如我们所报道的那样,为了在VATS肺叶切除术中实现完整的淋巴结清扫,我们可以完成左肺下叶袖式切除术,而保留左肺上叶[15](图4)。对于伴有N1淋巴结融合或叶间淋巴结侵犯支气管的左肺下叶肺癌患者而言,可采用全肺切除术[16]或舌段切除、左下叶袖式切除术[17]。
总结
对于可以通过微创技术治疗的具有挑战性的可切除NSCLC患者,应仅限于具有丰富VATS经验的大容量医学中心。对于中心型肺癌或者有淋巴结转移伴囊外侵犯的患者行VATS手术,要求术者具备预防和处置术中并发症的能力。只要有可能完成,我们强烈建议进行VATS手术。
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ettinger DS, Akerley W, Borghaei H, et al. Non-small cell lung cancer, version 2.2013. J Natl Compr Canc Netw 2013;11:645-53. [Crossref] [PubMed]
- Villamizar NR, Darrabie MD, Burfeind WR, et al. Thoracoscopic lobectomy is associated with lower morbidity compared with thoracotomy. J Thorac Cardiovasc Surg 2009;138:419-25. [Crossref] [PubMed]
- Paul S, Altorki NK, Sheng S, et al. Thoracoscopic lobectomy is associated with lower morbidity than open lobectomy: a propensity-matched analysis from the STS database. J Thorac Cardiovasc Surg 2010;139:366-78. [Crossref] [PubMed]
- Pischik VG. Technical difficulties and extending the indications for VATS lobectomy. J Thorac Dis 2014;6:S623-30. [PubMed]
- Hanna JM, Berry MF, D’ Amico TA. Contraindications of video-assisted thoracoscopic surgical lobectomy and determinants of conversion to open. J Thorac Dis 2013;5:S182-9. [PubMed]
- Berry MF, Onaitis MW, Tong BC, et al. Feasibility of hybrid thoracoscopic lobectomy and en-bloc chest wall resection. Eur J Cardiothorac Surg 2012;41:888-92. [Crossref] [PubMed]
- Grunenwald D, Spaggiari L. Transmanubrial osteomuscolar sparing approach for apical chest tumors. Ann Thorac Surg 1997;63:563-6. [Crossref] [PubMed]
- Soultanis KM, Chen Chao M, Chen J, et al. Technique and outcomes of 79 consecutive uniportal video-assisted sleeve lobectomies. Eur J Cardiothorac Surg 2019;56:876-82. [Crossref] [PubMed]
- Tabutin M, Couraud S, Guibert B, et al. Completion pneumonectomy in patients with cancer: postoperative survival and mortality factors. J Thorac Oncol 2012;7:1556-62. [Crossref] [PubMed]
- Decaluwe H, Sokolow Y, Deryck F, et al. Thoracoscopic tunnel technique for anatomical lung resections: a ‘fissure first, hilum last’ approach with staplers in the fissureless patient. Interact Cardiovasc Thorac Surg 2015;21:2-7. [Crossref] [PubMed]
- Amore D, Casazza D, Imitazione P, et al. Common and uncommon variations of pulmonary venous drainage in patients undergoing thoracoscopic lobectomy. Thorac Cardiovasc Surg 2019. [Epub ahead of print]. [PubMed]
- Li Y, Wang J. Analysis of lymph node impact on conversion of complete thoracoscopic lobectomy to open thoracotomy. Thorac Cancer 2015;6:704-8. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Is uniportal thoracoscopic surgery a feasible approach for advanced stages of non-small cell lung cancer? J Thorac Dis 2014;6:641-8. [PubMed]
- Fan J, Yao J, Wang Q, et al. Safety and feasibility of uniportal video-assisted thoracoscopic surgery for locally advanced non-small cell lung cancer. J Thorac Dis 2016;8:3543-50. [Crossref] [PubMed]
- Amore D, Casazza D, Bergaminelli C, et al. Left lower lobectomy and partial preservation of segmental arteries of left upper lobe: A strategy to avoid pneumonectomy in selected cases. Thoracic Cancer 2019;10:1837-40. [Crossref] [PubMed]
- Samejima J, Nakao M, Matsuura Y, et al. Prognostic impact of bulky swollen lymph nodes in cN1 non-small cell lung cancer patients. Jpn J Clin Oncol 2015;45:1050-4. [Crossref] [PubMed]
- Higuchi R, Nakagomi T, Shikata D, et al. Lingular segmentectomy and left lower lobectomy via unique bronchial dissection. J Thorac Dis 2018;10:E420-5. [Crossref] [PubMed]

薛家龙
医学硕士,上海市松江区中心医院胸外科医师。长期从事非小细胞肺癌的诊治,早期非小细胞肺癌的手术治疗等相关研究。参与辽宁省自然科学基金,先后发表中文核心论文数篇。(更新时间:2021/9/24)
(本译文仅供学术交流,实际内容请以英文原文为准。)
Cite this article as: Curcio C, Amore D, Casazza D, Saglia A, Imitazione P, Izzo A, Rispoli M, Nespoli MR. Thoracoscopic lobectomy for lung cancer in challenging cases: technical aspects. Curr Chall Thorac Surg 2019;1:25.



