
Surgical treatment for acquired tracheoesophageal fistula complicated with tracheal stenosis using endoscopic liner cutter staplers: a case report
Introduction
Acquired tracheoesophageal fistula (ATEF) is a rare clinical disease with a high case-fatality rate, which results from an abnormal communication between the trachea and esophagus due to some acquired factors (1-3). With complex and diverse etiologies, the clinical manifestations of ATEF are presented as the respiratory and digestive symptoms. We are reporting a case that a 43-year-old male with ATEF complicated with tracheal stenosis who received multiple treatments due to repeated stent displacement. We present the following case in accordance with the CARE reporting checklist (available at https://ccts.amegroups.com/article/view/10.21037/ccts-20-152/rc).
Case presentation
The patient, a 43-year-old male, was admitted to hospital with a history of ATEF for 2 years. He underwent pancreatoduodenectomy for pancreatic cyst 2 years ago and the resected specimens were reported to be benign by postoperative pathology. However, he was transferred to the intensive care unit (ICU) receiving tracheal intubation and mechanical ventilation for 20 days due to serious dyspnea following the pancreatoduodenectomy. One month after being discharged from hospital, the patient suffered from shortness of breath, dyspnea, nausea and vomiting with no obvious inducement. After hospitalization, the patient was diagnosed to suffer ATEF and received tracheal stent implantation and the fistula repair with endoscope. Then, he was discharged from hospital after the symptoms improved. However, in recent 2 years, the patient received the adjustment of implanted tracheal stent in hospital several times due to the stent displacement, and the digestive and respiratory symptoms still remained recurring.
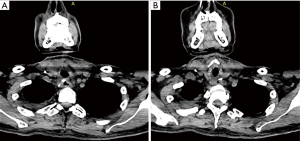
The relevant auxiliary examinations were performed after admission. Chest computed tomography (CT) examination and three-dimensional reconstruction of trachea both showed the changes with tracheal stent implantation, and the existence of ATEF complicated with trachea stenosis (Figure 1). Fiberoptic bronchoscope showed that there existed ATEF whose size was 1.0 cm × 1.5 cm (Figure 2). After preoperative evaluation based on relevant examination, the degree of trachea stenosis in the case was evaluated to be between 2/3 and 3/4, which indicated that the internal diameter of the narrow trachea was just 1/4 to 1/3 of the internal diameter of normal tracheas. Consequently, the patient was considered to require tracheal reconstruction.


In the preoperative period of our surgery, the dyspnea of the patient was so severe that the patient could not lie down and fall asleep for more than 2 hours at night in 20 days. Finally, based on the relevant examination and the patient’s condition, one-stage surgical treatment was decided. Endoscopic liner cutter staplers were applied to close the fistula and resect the narrow trachea directly, then tracheal reconstruction was conducted.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Findings in the surgery
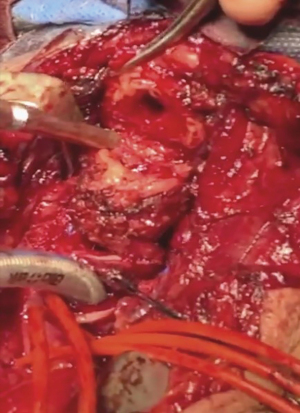
The length of subglottic stenosis reached 3 cm and the thyroid cartilage intima had proliferated and thickened seriously (Figure 3). The tracheal stent had moved down and obstructed unilateral main bronchi, and the ventilation function of the obstructed main bronchi totally depended on the fistula. The fistula with a size of 1.0 cm × 1.5 cm was observed to be 2 cm away from thyroid cartilage. There existed serious adhesion, degeneration and fusion between the esophagus and trachea at the upper edge of the fistula.
Steps of the surgery
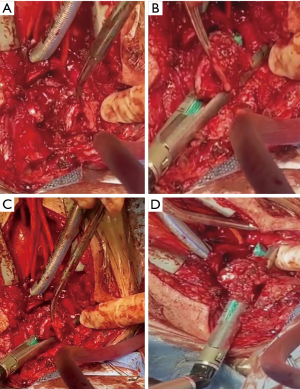
After the median incision of the upper one third of the sternum, the rest of sternum was cleaved obliquely to the right side Then the esophagus and trachea were exposed well after dissection. And it was observed that there existed serious adhesion and the abnormal structure between the esophagus and trachea at the upper edge of the fistula, which caused that it was difficult to separate away the esophagus and trachea in the dissection. Therefore, part of thyroid cartilage and thyroid cartilage intima were resected, and the cartilage rings of the narrow trachea were cut open from the front side to expand it for the expose of the fistula filed. Then the narrow trachea as well as the nearby esophagus were lifted in order to create the space for the application of endoscopic liner cutter staplers. However, the distance and space near the fistula were still not enough for endoscopic liner cutter staplers. Consequently, after adjusting the angle of placement, endoscopic liner cutter staplers were used to close the fistula with its nearby thickened tissues and cut the narrow trachea away (Figure 4). Finally, the mattress suture was applied to strengthen stapling of the fistula with VCP771D 4-0 (Figure 5).
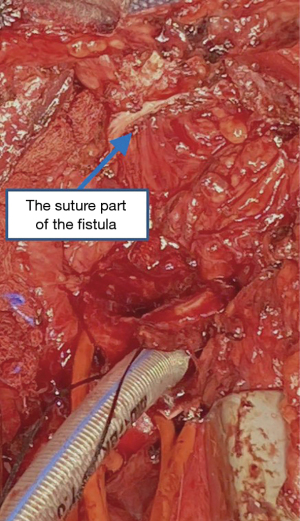
In this case, there existed thickened thyroid cartilage intima and subglottic stenosis. Therefore, the thickened thyroid cartilage intima was cut away in the reconstruction of airway. And the internal diameter of thyroid cartilage was dilated slowly and vigorously with hemostatic forceps in order to be anastomosed with the lower incisal edge of the trachea, whose structure was normal. After the completion of the reconstruction of airway, a pedicled thymus flap was used to surround the anastomosis in order to isolate the reconstructed trachea from the esophagus. In this way, the sutured part of the fistula could be covered firmly as well, which reduced the postoperative recurrence risk of ATEF.
The surgery was successful. The fistula was closed firmly through endoscopic liner cutter staplers. After the resection of the narrow trachea, the trachea and thyroid cartilage were anastomosed satisfactorily and the airway was reconstructed successfully. Finally, a tracheal cannula was applied for assisted ventilation.
Postoperative follow-up
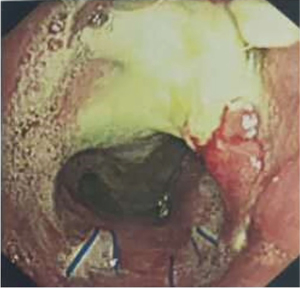
The patient recovered well without dyspnea, shortness of breath, cough, expectoration and other discomfort after the surgery. Fiberoptic bronchoscope was conducted 1 month later and showed normal postoperative changes of ATEF and no recurrence of ATEF (Figure 6); After 3 months, the chest CT and three-dimensional reconstruction of trachea were both conducted and showed slight stenosis above the tracheal anastomosis and no recurrence of ATEF (Figure 7).
Discussion
Surgical treatment is considered to be the first choice for ATEF. However, the recurrence rate remains high and it is very difficult to perform reoperation. Typically, the segmental resection and reconstruction of tracheas combined with double-layer suture of the esophageal defect is the standard surgery for ATEF with a diameter lager than 1 cm (4). For ATEF with a diameter less than 1 cm, the surgery that incise the fistula and repair trachea and esophagus respectively is often adopted to keep the integrity of respiratory and digestive tract. In addition, other surgical methods, such as the “double patch” technique proposed by Yang et al. (5,6), are also feasible, but the tracheal and esophageal reconstruction is required.
Postoperative traumatic ATEF is often associated with tracheal stenosis (7). The tracheal mucosae are pressed constantly by long-time tracheal intubation, which leads to the ischemia and necrosis of tracheal mucosae as well as the proliferation of granulation tissues and results in tracheal stenosis finally. For ATEF, it is necessary to pay attention to whether there exists tracheal stenosis. Before surgery, fiberoptic bronchoscopy, chest CT examination and three-dimensional reconstruction of trachea should be performed to analyze the degree and aggravation trend of tracheal stenosis. If the degree of tracheal stenosis is over 1/2, which indicates the internal diameter of the narrow trachea is less than 1/2 of the internal diameter of normal trachea, the tracheal reconstruction should be operated. And it should be considered to decide to resect partial trachea and reconstruct airway in a one-stage surgery, or choose to reconstruct airway in a more complicated and difficult two-stage surgery.
In this case, the patient was with a long course of ATEF complicated with tracheal stenosis. Resulting from long-term infection and inflammation in the fistula, there existed degeneration, hyperplasia, edema and necrosis in the tissues near the fistula. With high postoperative recurrence risk of ATEF, the regular surgical method that cut away the necrotic tissues of fistula and stitch the fistula directly is not reliable. Instead, endoscopic liner cutter staplers can be used to close the fistula more firmly, which not only benefits the retainment of the structure and function of the esophagus, but also reduces the risk of postoperative esophageal stenosis as well as the postoperative recurrence risk of ATEF. The application of endoscopic liner cutter staplers is considered to be the innovation of our surgery and the advantages were as following: (I) the cutting and stapling are carried out concurrently through endoscopic liner cutter staplers, which reduces intraoperative contamination from infected fistula and it nearby tissues; (II) the application of endoscopic liner cutter staplers simplifies surgical procedure, preserves the integrity of digestive tract, and avoids the esophageal reconstruction (7).
In the reconstruction of the patient’s airway, the management of the thickening parts and stenosis of thyroid cartilage intima was just trimmed instead of being resected totally. Moreover, the postoperative patency of the airway depended on the situation of pathological changes of trachea. Therefore, the tracheal stenosis might reoccur after the airway reconstruction. In case that laryngeal edema or bilateral recurrent laryngeal nerve injury might occur after the operation and result in dyspnea, it was necessary to apply a tracheal cannula for assisted ventilation.
Conclusions
For this patient with ATEF complicated with tracheal stenosis, it was difficult to separate away the trachea and esophagus near the upper edge of the fistula in the dissection. Therefore, the cartilage rings of the narrow trachea were cut open from the front side and the narrow trachea as well as the nearby esophagus were lifted in order to create the enough space for application of endoscopic liner cutter staplers. After adjusting the angle of placement, endoscopic liner cutter staplers were used to close the fistula with the its nearby thickened tissues, and cut the narrow trachea away. Finally, after resection of the narrow trachea, the trachea and thyroid cartilage were anastomosed to reconstruct the airway. A tracheal cannula was applied for assisted ventilation finally. Our surgical method was proved to be simple and effective in the postoperative follow-up of the patient.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Tutku Soyer) for the series “Tracheoesophageal Fistula” published in Current Challenges in Thoracic Surgery. The article has undergone external peer review.
Reporting Checklist: The authors have completed the CARE reporting checklist Available at https://ccts.amegroups.com/article/view/10.21037/ccts-20-152/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ccts.amegroups.com/article/view/10.21037/ccts-20-152/coif). The series “Tracheoesophageal Fistula” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Muniappan A, Wain JC, Wright CD, et al. Surgical treatment of nonmalignant tracheoesophageal fistula: a thirty-five year experience. Ann Thorac Surg 2013;95:1141-6. [Crossref] [PubMed]
- Muniappan A, Mathisen DJ. Repair of tracheo-oesophageal fistula. Multimed Man Cardiothorac Surg 2016;2016:mmw002. [Crossref] [PubMed]
- de Castro G, Iribarren M, Rivo E, et al. Tracheoesophageal fistula in an intubated patient. Treatment through exclusion and esophageal patch. Cir Esp 2005;77:230-2. [Crossref] [PubMed]
- Bibas BJ, Guerreiro Cardoso PF, Minamoto H, et al. Surgical Management of Benign Acquired Tracheoesophageal Fistulas: A Ten-Year Experience. Ann Thorac Surg 2016;102:1081-7. [Crossref] [PubMed]
- Yang G, Li WM, Zhao JB, et al. A novel surgical method for acquired non-malignant complicated tracheoesophageal and bronchial-gastric stump fistula: the "double patch" technique. J Thorac Dis 2016;8:3225-31. [Crossref] [PubMed]
- Yang G, Zhou YA, Bai GZ, et al. Effect of cauterizing esophageal mucosa in "double-patch" treatment for acquired benign tracheoesophageal fistula/bronchogastric stump fistula. J Surg Res 2017;209:1-7. [Crossref] [PubMed]
- Yang GY. Direct closure and isolation of benign acquired tracheoesophageal fistula in the treatment of 2 cases. Journal of Chinese Practical Diagnosis and Therapy 2018;32:209-10.
Cite this article as: Yang G, Xian L, Zhao W, Huang C, Liang X, Sun Y, Yang S, Liu W, Bi X, Liang F, Wang M, Chen Y, Lu Y. Surgical treatment for acquired tracheoesophageal fistula complicated with tracheal stenosis using endoscopic liner cutter staplers: a case report. Curr Chall Thorac Surg 2021;3:41.


