Decortication of fibrous pleural rind by uniportal video-assisted thoracic surgery in patients with tuberculous empyema
Introduction
Stage III tuberculous empyema often occurs due to the failure to receive timely treatment for stage I and stage II tuberculous empyema. The most important feature of stage III tuberculous empyema is the fibrous peel covering the visceral and parietal pleura. The long-term, chronic presence of a fibrous peel can not only compress the lung, making it unable to completely expand, but can lead to thoracic deformation and even scoliosis. When empyema reaches this point, its course is difficult to reverse with drug treatment, and decortication of the fibrous peel is necessary to allow the lung to expand (1). Additionally, thorough visceral fibrous peel decortication can often greatly improve the deformation of the chest. Conventional fibrous peel decortication is often performed via thoracotomy. With the progress of thoracoscopic technology, fibrous peel decortication can also be completed under endoscopy. At present, Kumar (2) has published the largest number of reports in the world. He reported 100 cases of stage III tuberculosis with empyema treated with decortication of the fibrous pleural peel under thoracoscopy. In his report, severe stenosis of the intercostal space and calcification plate formation were considered to be relative contraindications for thoracoscopy. However, in recent years, uniportal thoracoscopy has gradually become a mature thoracoscopy technology, and increasingly difficult surgeries can be completed through this method (3). Therefore, we attempted to apply the uniportal endoscopic technique to difficult fibrous peel decortication in a patient with empyema.
Case presentation
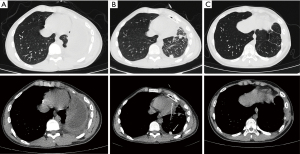
A 17-year-old male was diagnosed with left tuberculous empyema due to progressive shortness of breath. During 4 months of anti-tuberculosis treatment, he experienced two closed thoracic drainage placements with poor results. Computed tomography (CT) performed on admission showed left encapsulated pleural effusion and obvious left intercostal space stenosis accompanied by the left thoracic collapse (Figure 1).
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s parent or legal guardian for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Surgical technique
Double lumen tube intubation was used for anesthesia, and patient was placed in the lateral position, which was the same position used for conventional thoracic surgery. For the incision, based on the preoperative CT findings, the deepest layer of the abscess cavity was selected. In this case, we selected the midline of the seventh axillary rib and made a 6-cm incision there, then opened the incision layer by layer down to the rib surface, electrocoagulated and cut the periosteum on the rib surface, stripped the periosteum of the rib 6 cm below the incision with a periosteal stripper to preserve as much as of the periosteum as possible, and then resected the rib 6 cm below the incision in segments to obtain an operational space approximately 1.5 cm wide. We then used fingers to bluntly separate the gap between the parietal fibrous peel and the chest wall. Then, the space was tightly packed with gauze for approximately 5 minutes for compression and to stop the bleeding. After all of the gauze was removed, a wound protective sleeve was placed in the incision. The thoracoscope was then placed to check for obvious bleeding points on the side of the parietal pleura. If there were bleeding points, electrocoagulation was used to stop the bleeding. At this time, the incision was completed (Figure 2).
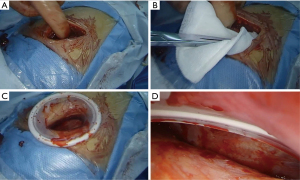
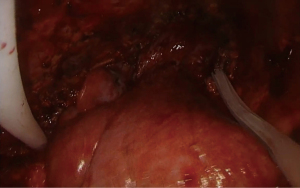
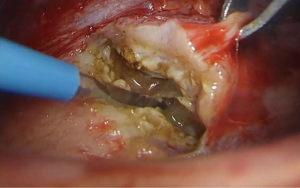
After the incision was completed, it was completely sterilely enclosed by the protective sleeve, which was kept in place until the end of the operation. Then, an electric knife was used to cut the parietal fibrous peel below the incision and enter the abscess cavity. The contents of the abscess cavity were collected and submitted for inspection as quickly possible. The parietal fibrous peel was then gradually removed to create a fenestration in the abscess cavity below the incision, the contents of the abscess cavity were cleared, and the entire abscess cavity was completely emptied (Video 1). At this point, the abscess cavity was exposed (Figure 3).
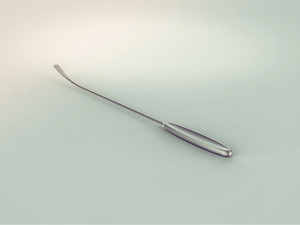
After the sharp incision of the visceral fibrous peel with the blade, we searched for the gap between the fibrous peel and the visceral pleura and started stripping the visceral fibrous peel from the lung with a patented extended stripper (Figure 4) after the appropriate plane was found. The separation of the visceral fibrous peel and the parietal fibrous peel was then performed alternately (Video 2). When the fibrous peel was separated at the turning point of the visceral parietal fibrous peel, the fibrous peel was thicker and could be cut with an electrocoagulation cutting (Video 3). The fibrous peel on the diaphragmatic surface could also be removed using the same blunt separation method combined with electric knife cutting. If the diaphragmatic surface was slightly damaged during separation, it could be closed by figure-of-eight suture (Video 4).
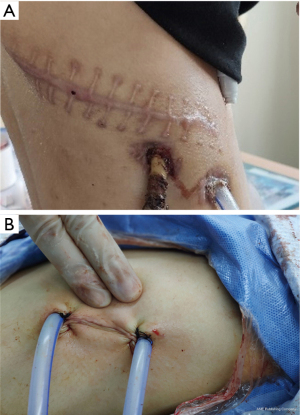
After all of the fibrous peels were stripped, the area was washed repeatedly and tested for leakage. Superficial contusions and lacerations on the lung surface did not need be treated. The chest tube was cross-placed with grooved tubes (Video 5), the protective sleeve was removed, and the bleeding of the incision was stopped. The groove tubes were placed backward along the front edge of the incision to the top of the abscess cavity and forward to the front and top of the abscess cavity at the rear edge of the incision (Figure 5). The muscles were sutured layer by layer. At that point, the operation was completed. The whole operation time is 4.5 hours and bloods was 400 mL.
Early mobilization and active breathing exercises was encouraged after the operation until the drainage flow was less than 50 mL/day 1 week after the operation and there was no air leakage. CT re-examination showed complete recruitment of the lung and disappearance of the residual cavity. At that time, the tube was removed, and anti-tuberculosis treatment was continued. The thoracic collapse was improved after 3 months (Figure 1).
Comments
Stage III tuberculous empyema often requires thorough decortication of fibrous peels to enable subsequent drug treatment to be effective and a cure to be achieved. Tuberculous empyema is a benign disease. Reducing the conventional thoracotomy incision to a 5- to 6-cm uniportal thoracoscopic incision can greatly reduce the surgical trauma (Figure 6). Especially for teenagers, who have not completed their development, thoracoscopic surgery can avoid the potential risk of future scoliosis caused by forced opening (4). A few reports of uniportal empyema treatment indicate that this technique is usually applied to stage I and stage II empyema (5,6). Additionally, in previous reports of empyema surgery, severe stenosis of the intercostal space (Figure 1) is considered a contraindication for thoracoscopic surgery (1,7,8). This early case report from our center broke from this contraindication and confirmed that this technology is safe and reliable (9). This study further summarizes a mature surgical operation route. For patients whose intercostal space is often nearly closed, it is almost impossible for conventional endoscopy to enter the chest through the intercostal space. This is the reason that other studies believe that such patients are contraindicated for endoscopic surgery. We performed segmental rib resection to obtain an operation gap at least 1–1.5 cm wide. The rib resection length was generally 5–6 cm. Such a defect does not affect the integrity of the thorax but allows full use of the extent of the protective sleeve. Due to the limitation of using a single hole, the decortication of fibrous peels needs to be completed using instruments with a long handle and radian. We designed a special lengthened periosteal stripper for this purpose. The fibrous peels and visceral pleura of some patients are closely bonded, and it is difficult to avoid damaging the visceral pleura during stripping. Superficial lacerations are left open and close naturally with later lung recruitment. The removal of parietal fibrous peels is the key to enabling the abnormal thorax to recover as soon as possible. When stripping off the parietal fibrous peel, we prioritize blunt separation, combined with electrocoagulation separation. Due to the limitations of the incision, the visceral fibrous peel and the parietal fibrous peel are gradually removed in small pieces. Two chest tubes are used for drainage. One chest tube is placed from the front edge of the incision and extends along the posterior mediastinum to the upper back of the empyema, and the second chest tube is placed from the rear edge of the incision to the upper front of the abscess cavity. With the use of special instruments, uniportal thoracoscopy is safe and feasible for total fibrous peel decortication in patients with stage III tuberculous empyema. Combined with standardized postoperative anti-tuberculosis treatment, the long-term recovery effect is good.
Acknowledgments
We thank all of the staff of the operating room and the anesthesiology department for their efforts.
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by Dr. Gening Jiang, Editor-in-Chief of the journal Current Challenges in Thoracic Surgery. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ccts.amegroups.com/article/view/10.21037/ccts-21-40/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s parent or legal guardian for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Shaw JA, Irusen EM, Diacon AH, et al. Pleural tuberculosis: A concise clinical review. Clin Respir J 2018;12:1779-86. [Crossref] [PubMed]
- Kumar A, Asaf BB, Lingaraju VC, et al. Thoracoscopic Decortication of Stage III Tuberculous Empyema Is Effective and Safe in Selected Cases. Ann Thorac Surg 2017;104:1688-94. [Crossref] [PubMed]
- Soultanis KM, Chen Chao M, Chen J, et al. Technique and outcomes of 79 consecutive uniportal video-assisted sleeve lobectomies. Eur J Cardiothorac Surg 2019;56:876-82. [Crossref] [PubMed]
- Feiz HH, Afrasiabi A, Parvizi R, et al. Scoliosis after thoracotomy/sternotomy in children with congenital heart disease. Indian J Orthop 2012;46:77-80. [Crossref] [PubMed]
- Ismail M, Nachira D, Meacci E, et al. Uniportal video-assisted thoracic surgery in the treatment of pleural empyema. J Thorac Dis 2018;10:S3696-703. [Crossref] [PubMed]
- Elkhayat H. Uniportal VATS approach for treatment of empyema: Challenges and recommendations. Multimed Man Cardiothorac Surg 2018; [Crossref] [PubMed]
- Ju J, Duan L, Yu G, et al. Video-assisted small-incision decortication in the treatment of adolescent organized tuberculous empyema: a 26-case report. Chinese Journal of Thoracic and Cardiovascular Surgery 2017;33:601-2.
- Tang W, Wang S, Chen C, et al. Uniportal thoracoscopic fibrous pleural plate debridement in 21 cases of encapsulated tuberculous chest abscess. Chinese Journal of Thoracic and Cardiovascular Surgery 2015;31:425, 430.
- Zhou Y, Li X, Dai J, et al. Uniportal Thoracoscopic Decortication for Stage III Tuberculous Empyema With Severe Rib Crowding. Ann Thorac Surg 2021;112:289-94. [Crossref] [PubMed]
Cite this article as: Cai H, Mao R, Yin G, Zhou Y. Decortication of fibrous pleural rind by uniportal video-assisted thoracic surgery in patients with tuberculous empyema. Curr Chall Thorac Surg 2022;4:21.