
Uniportal video-assisted thoracoscopic surgery for lung cancer—current practices and outcomes: a narrative review
Introduction
Over the last two decades, video-assisted thoracoscopic surgery (VATS) has evolved from a procedure primarily carried out for diagnostic purposes to one most often performed with therapeutic intent. In fact, even prior to the acquisition of high-level scientific evidence supporting its use, minimally invasive surgery became the recommended approach for the treatment of early-stage lung cancer (1). A recent randomized trial was initiated to verify that VATS offers superior postoperative clinical outcomes and similar early oncologic outcomes when compared with lobectomy via thoracotomy (2). The 1-year results from this trial confirmed the superiority of VATS lobectomy over open thoracotomy lobectomy for better clinical outcomes, both early postoperatively and 1 year after lobectomy, with no differences in disease-free and overall survival between the 2 approaches (3).
Despite slow adoption initially (4), VATS lobectomy is now regarded as a universal, feasible, and safe procedure that is associated with decreased postoperative pain and morbidity and faster recovery (2,5-7). The advent of sophisticated dissection tools and high-resolution camera technology, along with the natural surgeon’s instinct to push boundaries, has resulted not only in implementation of minimally invasive surgery but also adoption of innovations as to decrease the number of incisions even when performing complex VATS anatomic lung resections (8,9).
VATS lobectomy has been most often performed via 2 to 4 incisions (10,11). However, in 2004, Rocco and colleagues (12) introduced the concept of the uniportal approach (one incision in one intercostal space), and in 2011, Gonzalez–Rivas and colleagues published the first case report of uniportal VATS (U-VATS) lobectomy for an early-stage lung cancer (13). Over the last decade, several European and Asian thoracic surgeons have published details and outcomes of complex resections via this uniportal approach including segmentectomy, pneumonectomy, and sleeve and double-sleeve lung resections (14-17). Yet, despite multiple series showing that uniportal VATS lobectomy is at least equivalent to multiport VATS (M-VATS) lobectomy when considering perioperative outcomes and possibly has advantages of better pain control and shorter hospital stay (18), thoracic surgeons in North America are still reluctant to adopt the U-VATS approach (19). Interestingly, Yu and colleagues recently published their results of a prospective trial comparing M-VATS and U-VATS and showed less immunomodulatory chemokine production, namely less tissue inhibitor of matrix metalloproteinase (TIMP)-1 and matrix metalloproteinase (MMP)-9 production, in the U-VATS group (20). These findings raise the question of whether U-VATS may, in fact, be a less aggressive approach. Although U-VATS is a promising and innovative approach, data on long-term oncologic outcomes after U-VATS resection are still scarce. Nonetheless, the lessons learned from experience with M-VATS lobectomy can be applied to further improve clinical and oncological outcomes of the uniportal VATS approach.
From this perspective, we aim to review the surgical outcomes of uniportal VATS lobectomy and describe our institutional experience, highlighting current practices that may facilitate the adoption of U-VATS. We present this article in accordance with the Narrative Review reporting checklist (available at https://ccts.amegroups.com/article/view/10.21037/ccts-21-38/rc).
Methods
We performed PubMed and Google Scholar searches using the following keywords: lung cancer, video-assisted surgery, single-port surgery, VATS, U-VATS, and uniportal thoracic surgery. All articles in English published from 2000 to 2021 were reviewed to elaborate this manuscript. Randomized clinical trials, meta-analysis and multicenter studies were prioritized and read in full. Table 1 details the search strategy summary in full. Also, we detailed our institutional practices for performing U-VATS and caring for patients undergoing U-VATS lobectomy with an Enhanced Recovery Protocol.
Table 1
| Items | Specification |
|---|---|
| Date of search | January 1st, 2021 |
| Databases and other sources searched | PubMed, Google Scholar |
| Search terms used | Search terms: lung cancer, video-assisted surgery, single-port surgery, VATS, U-VATS, and uniportal thoracic surgery |
| Timeframe | From January 1st, 2000 to January 1st, 2021 |
| Inclusion and exclusion criteria | Inclusion criteria: (I) U-VATS surgery (segmentectomy, lobectomy, pneumonectomy); (II) article languages: English; (III) article types: randomized clinical trials, meta-analysis, and multicenter studies. Exclusion criteria: None |
| Selection process (who conducted the selection, whether it was conducted independently, how consensus was obtained, etc.) | All abstracts were read in full by FSW and CAM; relevant studies were read in full by FSW; all major studied were brought to the attention of all co-authors to be hand-picked by consensus |
| Example of the search strategies used in PubMed | (Single port or uniport*) AND lung surgery; U-VATS; single port VATS; video-assisted thoracoscopy |
VATS, video-assisted thoracoscopic surgery; U-VATS, uniportal VATS.
Discussion
Institutional protocols
Preoperative care
In 2008, our institution adopted a Rapid Diagnostic Assessment Program (DAP) to promote a homogenous pattern of patient care from diagnosis to treatment. Cancer staging tests and preoperative evaluation include pulmonary function tests, cardiac evaluation, bronchoscopy, chest computed tomography (CT) scan, positron emission tomography (PET) scan, brain imaging and lung or lymph node biopsy for diagnosis (21). Endobronchial ultrasound (EBUS) is ordered according to the European Society of Thoracic Surgery (ESTS) criteria for invasive mediastinal staging (22). All patients receive education on lung cancer and smoking cessation counseling. Table 2 summarizes the different steps of the patient’s clinical care trajectory.
Table 2
| Preoperative strategies |
| Preoperative visit, evaluation, and investigations with accelerated DAP |
| Patient education, smoking cessation, preoperative workout plan, and explanation of the ERP |
| Same-day admission |
| Perioperative strategies |
| Antibiotic and venous thromboembolism prophylaxis |
| Regional anesthesia as needed |
| Goal-directed fluid therapy |
| Minimally invasive surgery (VATS) |
| Single chest drainage |
| Postoperative strategies |
| Avoidance of opiates |
| Avoidance of intravenous fluid overloading |
| Early ambulation, feeding and physiotherapy |
| Rapid-recovery-directed nursing |
| Early removal of chest tubes |
| Postoperative education |
| Booklet about postoperative care |
| Rapid, elective, clinical reassessment |
DAP, diagnostic assessment program; ERP, enhanced recovery protocol; VATS, video-assisted thoracoscopic surgery.
In conjunction with the DAP, an institutional enhanced recovery protocol (ERP) that consists of a well-structured plan to educate patients and caregivers preoperatively and postoperatively was implemented (21). The European Society of Thoracic Surgeons (ESTS) has published guidelines for fast-track postoperative care of lung cancer patients treated surgically (23), and we follow their recommendations for enhanced recovery. According to their guidelines, prior to surgery, patients receive dedicated counseling and are screened for nutritional status. Malnourished patients can benefit from nutritional counseling and supplements. Smoking and alcohol cessation is strongly advised to start at least 4 weeks prior to intervention. Lastly, in patients with borderline lung function, pulmonary rehabilitation is encouraged despite low-level evidence supporting this recommendation. Routine administration of sedatives preoperatively is discouraged (Table 2). These enhanced recovery protocols and guidelines have a positive influence on patient outcomes (24).
Intraoperative—uniportal VATS lobectomy institutional approach
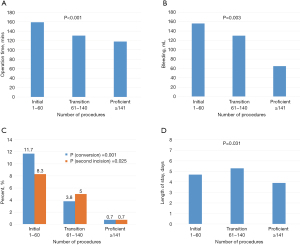
Our adoption of the U-VATS approach in 2014 was carefully planned (Figure S1). We developed a prospective database and a strategy to record and review our surgeries so constant adjustments to the technique could be implemented. Naturally, at the beginning, surgeries were longer, and we incurred in higher rate of vascular accidents and conversions to M-VATS or thoracotomy (25). We recently published our U-VATS learning curve, in which we identified 3 different phases according to number of procedures performed within each timeframe. The initial phase consisted of 60 lobectomies, followed by a transition phase of up to 140 lobectomies before the proficient phase was reached. Within each phase, we analyzed surgical time, blood loss, conversion rate to thoracotomy and the need for a second incision as well as other variables (26) (Figure 1). Others have also published on the learning curve of U-VATS lobectomy, and most agree that this approach involves a steep learning curve (27-31).
At our center U-VATS lobectomy is performed with the patient under general anesthesia and with single-lung ventilation. The patient is positioned in full lateral decubitus with flexion of the table at the level of the mid-chest, allowing slight widening of the intercostal space that will improve exposure and facilitate access to the pleural cavity. In 2019, the ESTS Uniportal VATS Interest Group, published a consensus report on standardization of the uniportal technique for lobectomy describing precisely how experts perform the procedure. It was agreed that the maximum incision size should be 4 cm, that the incision should be made between the middle and anterior axillary lines, and that a wound retractor could be employed but rib spreading must not be used. Either a 10-mm camera or a 5-mm camera is acceptable, though the procedure is probably easier with the smaller camera. Additionally, only 1 chest tube, 28 French or smaller and placed through the same skin incision, should be used, and either intercostal or paravertebral nerve blocks are the preferred analgesia (32).
Once the pleural space is entered, a thorough exploration is performed to confirm resectability. The sequence of dissection for most lobectomies is as follows: (I) for right upper lobectomy—arteries, bronchus, then vein; (II) left upper lobe and right and left lower lobes—arteries, vein, then bronchus, and (III) for the right middle lobe—vein, bronchus, then arteries. We perform hilar and lobe-guided mediastinal lymphadenectomy in all patients. We spend time to thoroughly expose all elements of the hilum, because we believe this is crucial to perform a safe operation. After complete removal of the hilar and lobar lymph nodes, the lobar vessels are well exposed. Each vessel is then dissected at its base, in the periadventitial plane and with no tension. We prefer to use an endostapler with curved-tip cartridges to transect all vascular branches. Once all peribronchial lymphatic tissue is swiped towards the specimen, we transect the bronchus with a thick stapler load. For the dissection of the parenchyma, we generally will use a medium-thick load; however, for emphysematous patients, we favor the reinforced reload.
Only patients with impaired pulmonary lung function will require an epidural catheter. Otherwise, we perform preemptive analgesia through intercostal nerve block with bupivacaine prior to incision. We perform a second round of intercostal nerve block from the intrapleural space prior to removal of the specimen. We insert a 24-French chest tube through the single surgical incision at closure (Figure 2).

Postoperative care
Most patients will recover for the first 24 h after surgery in a step-down unit. Only high-risk patients or patients undergoing major lung resections, such as pneumonectomy, will recover in the intensive care unit. According to our institutional postoperative care enhanced recovery protocol, patients are mobilized 4 h after surgery to a chair, and walking is encouraged under supervision soon after. Respiratory physiotherapy exercises are taught as soon as the patient is well awake and are practiced regularly with the help of the nursing staff, physiotherapists, and family members. We strongly support the participation of family in our patients’ care as they will be the primary caregivers after discharge (Table 2). For pain control, we use a combination of oral acetaminophen and a patient-controlled analgesia (PCA) pump that contains hydromorphone. A single chest tube under a water seal is generally used for drainage. Chest tubes are removed as soon as possible as long as there is no air leak and drainage is <300 mL in 24 h. Discharge is usually prior to postoperative day 3, but as a referral center for the province, patients from distant sites may be dependent on transfers and require a longer stay. Follow-ups at an outpatient clinic are scheduled 2 weeks following discharge. At this follow-up appointment, the pathology report will be reviewed with the patient and family to determine the next steps in treatment.
Surgical outcomes of U-VATS vs. M-VATS
Postoperative pain
Two systematic reviews with meta-analysis have been published comparing postoperative pain after U-VATS and M-VATS. The first, in 2018 by Yang and colleagues (33), pooled the results reported in 3 articles (34-36) and found significantly lower pain, assessed using a visual analog scale, on postoperative day 1 after U-VATS as compared with M-VATS, while reporting no difference 72 h after surgery in 2 of the 3 studies (34,35). The second meta-analysis, published by Ng and colleagues in 2019 (37), was a pooled analysis of 2 articles (34,38) and again revealed that patients who underwent U-VATS had significantly lower visual pain scores on postoperative day 1, as well as on postoperative days 3, 7 and 30, than patients who underwent M-VATS.
Several retrospective and single-institution series have also examined pain after U-VATS as compared with M-VATS. Wang and colleagues (39) compared U-VATS with M-VATS and with open thoracotomy. The patients who underwent U-VATS had significantly lower visual pain scores as compared with the other two groups 1, 2, and 3 days postoperatively and pain scores were still significantly lower 1 week and 1 month postoperatively. Zhao and colleagues (40) also compared the three techniques, but focused on elderly patients, and again found that the U-VATS group had significant lower pain scores on postoperative days 1 and 3 and on the last day of hospital stay, when pain was evaluated as part of a patient global assessment. Furthermore, Abouarab, Yan, and Louis with their colleagues have all shown that patients who undergo U-VATS for lobectomy and sublobar resection take significantly less pain medication, including narcotics, when compared with patients who undergo M-VATS resections (41-43). Conversely however, in 2019, Tosi and colleagues (44), using the Italian VATS Group database, reported that U-VATS patients had a significantly higher level of pain on postoperative days 2 and 3 than M-VATS patients. In our opinion after using U-VATS for several years, uniportal VATS generally results in less postoperative pain, because only one incision is used instead of the 2–4 incisions typical for M-VATS. With fewer incisions, we believe there is less chance of damaging multiple intercostal nerves and less chance of acute and chronic postoperative pain.
Length of stay (LOS) and duration of chest tube drainage
Three meta-analyses of LOS and duration of chest tube placement after U-VATS with conflicting results have been published. In 2020, Yan and colleagues included 20 papers for a total of 4,142 patients in their meta-analysis and examined perioperative and early postoperative outcomes of U-VATS versus M-VATS. Length of stay was reported in 12 studies for a total of 2,490 patients, and duration of drainage was reported in 18 studies for a total of 2,743 patients. Yan observed statistically similar LOS between groups (5.7±4.0 U-VATS and 7.2±5.1 M-VATS) and similar chest tube duration between groups (3.9±2.9 days U-VATS and 4.4±3.1 days M-VATS) (42). Two earlier meta-analyses also showed significantly shorter LOS and chest tube duration in the U-VATS group as compared to with M-VATS group (41,45).
Other complications
Other factors, such as blood loss, complication rate, and number of resected lymph nodes have also been evaluated when comparing U-VATS and M-VATS. The number of resected lymph nodes did not vary between the 2 approaches in any of the meta-analyses detailed above. Blood loss and complication rate after U-VATS were similar to or better than after M-VATS depending on the meta-analysis, indicating favorable outcomes after U-VATS in both the treatment of minor and major lung disorders (41,42,45). Our group recently compared the early postoperative outcomes after U-VATS lobectomy as compared with M-VATS lobectomy for non-small cell lung cancer. Although patients who underwent U-VATS had a lower rate of postoperative pneumonia and air leakage in a multivariable analysis, no significant differences in the complication rate were observed in a propensity-matched analysis. Furthermore, the conversion-to-thoracotomy rate, the need for a transfusion, and the harvesting of lymph nodes were all similar between the 2 approaches. The U-VATS approach showed a shorter surgical time and less intraoperative bleeding. This study revealed that, in hands of experts, U-VATS has similar surgical outcomes as M-VATS (46). Abouarab and colleagues (41) also reported that U-VATS and M-VATS have similar rates of postoperative complications. A systematic review with meta-analysis (37) found a significant lower rate of overall postoperative complications, such as prolonged air leak and pneumonia in patients undergoing U-VATS as compared with M-VATS when assessing 6 studies for a total of 1,010 patients. Finally, a randomized trial comparing U-VATS and M-VATS for lobectomy showed no statistically significant differences in perioperative and early postoperative outcomes including postoperative pain, LOS, chest tube duration and 30-day mortality (47).
U-VATS limitations
There are some limitations to U-VATS currently. U-VATS is one of the most recently developed VATS techniques and may have a steeper learning curve than M-VATS. Unfortunately, high-quality data on oncological outcomes is scarce, and several surgeons do not believe that decreasing the number of incisions will translate into a clinical advantage for patients (26). A key question is, how much energy should we devote to changing our approach in the absence of scientific proof of superiority? Some believe this is a futile matter.
To our knowledge, no prospective or randomized trial has demonstrated superiority of U-VATS over M-VATS, in the meantime, VATS approaches with 2 to 4 incisions are well-accepted approaches to VATS lobectomy, which has been proven superior to thoracotomy for early-stage lung cancer.
Conclusions
The use of enhanced recovery protocols and guidelines for lung cancer management is key to provide the best care for patients and allow them a faster return to their normal life (24). Recent studies suggest that U-VATS is less invasive and is associated with less production of immunomodulatory chemokines and fewer postoperative complications while delivering comparable oncological results as M-VATS. As the adoption of U-VATS approaches increases worldwide, we believe it is only a matter of time until stronger oncological data is published to further support the use of U-VATS. Additionally, we will only be able to properly teach U-VATS to junior surgeons after senior surgeons embrace the technique.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Jean Bussières and George Rakovich) for the series “Recent Advances in Perioperative Care in Thoracic Surgery and Anesthesia” published in Current Challenges in Thoracic Surgery. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://ccts.amegroups.com/article/view/10.21037/ccts-21-38/rc
Peer Review File: Available at https://ccts.amegroups.com/article/view/10.21037/ccts-21-38/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ccts.amegroups.com/article/view/10.21037/ccts-21-38/coif). The series “Recent Advances in Perioperative Care in Thoracic Surgery and Anesthesia” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ettinger DS, Wood DE, Akerley W, et al. Non-Small Cell Lung Cancer, Version 6.2015. J Natl Compr Canc Netw 2015;13:515-24. [Crossref] [PubMed]
- Lim E, Batchelor T, Shackcloth M, et al. Study protocol for VIdeo assisted thoracoscopic lobectomy versus conventional Open LobEcTomy for lung cancer, a UK multicentre randomised controlled trial with an internal pilot (the VIOLET study). BMJ Open 2019;9:e029507. [Crossref] [PubMed]
- Lim EKS, Batchelor TJP, Dunning J, et al. Video-assisted thoracoscopic versus open lobectomy in patients with early-stage lung cancer: One-year results from a randomized controlled trial (VIOLET). J Clin Oncol 2021;39:8504. [Crossref]
- Boffa DJ, Allen MS, Grab JD, et al. Data from The Society of Thoracic Surgeons General Thoracic Surgery database: the surgical management of primary lung tumors. J Thorac Cardiovasc Surg 2008;135:247-54. [Crossref] [PubMed]
- Stephens N, Rice D, Correa A, et al. Thoracoscopic lobectomy is associated with improved short-term and equivalent oncological outcomes compared with open lobectomy for clinical Stage I non-small-cell lung cancer: a propensity-matched analysis of 963 cases. Eur J Cardiothorac Surg 2014;46:607-13. [Crossref] [PubMed]
- Yang CJ, Kumar A, Klapper JA, et al. A National Analysis of Long-term Survival Following Thoracoscopic Versus Open Lobectomy for Stage I Non-small-cell Lung Cancer. Ann Surg 2019;269:163-71. [Crossref] [PubMed]
- Boffa DJ, Kosinski AS, Furnary AP, et al. Minimally Invasive Lung Cancer Surgery Performed by Thoracic Surgeons as Effective as Thoracotomy. J Clin Oncol 2018;36:2378-85. [Crossref] [PubMed]
- Huang J, Li J, Qiu Y, et al. Thoracoscopic double sleeve lobectomy in 13 patients: a series report from multi-centers. J Thorac Dis 2015;7:834-42. [PubMed]
- Chen HW, Du M. Video-assisted thoracoscopic pneumonectomy. J Thorac Dis 2015;7:764-6. [PubMed]
- Daniels LJ, Balderson SS, Onaitis MW, et al. Thoracoscopic lobectomy: a safe and effective strategy for patients with stage I lung cancer. Ann Thorac Surg 2002;74:860-4. [Crossref] [PubMed]
- McKenna RJ Jr, Houck W, Fuller CB. Video-assisted thoracic surgery lobectomy: experience with 1,100 cases. Ann Thorac Surg 2006;81:421-5; discussion 425-6. [Crossref] [PubMed]
- Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg 2004;77:726-8. [Crossref] [PubMed]
- Gonzalez-Rivas D, de la Torre M, Fernandez R, et al. Single-port video-assisted thoracoscopic left upper lobectomy. Interact Cardiovasc Thorac Surg 2011;13:539-41. [Crossref] [PubMed]
- Gonzalez-Rivas D, Fieira E, Delgado M, et al. Uniportal video-assisted thoracoscopic sleeve lobectomy and other complex resections. J Thorac Dis 2014;6:S674-81. [PubMed]
- Gonzalez-Rivas D. Single incision video-assisted thoracoscopic anatomic segmentectomy. Ann Cardiothorac Surg 2014;3:204-7. [PubMed]
- Vannucci F, Vieira A, Ugalde PA. The technique of VATS right pneumonectomy. J Vis Surg 2018;4:11. [Crossref] [PubMed]
- Royo-Crespo I, Vieira A, Ugalde PA. Extended uniportal video-assisted thoracic surgery for lung cancer: is it feasible? J Vis Surg 2018;4:57. [Crossref] [PubMed]
- Shen Y, Wang H, Feng M, et al. Single- versus multiple-port thoracoscopic lobectomy for lung cancer: a propensity-matched study†. Eur J Cardiothorac Surg 2016;49:i48-53. [PubMed]
- Yeung C, Gilbert S. The state of uniportal video-assisted thoracoscopic surgery in North America: a survey of thoracic surgeons. J Vis Surg 2018;4:19. [Crossref] [PubMed]
- Yu PSY, Chan KW, Lau RWH, et al. Uniportal video-assisted thoracic surgery for major lung resection is associated with less immunochemokine disturbances than multiportal approach. Sci Rep 2021;11:10369. [Crossref] [PubMed]
- Hubert J, Bourdages-Pageau E, Garneau CAP, et al. Enhanced recovery pathways in thoracic surgery: the Quebec experience. J Thorac Dis 2018;10:S583-90. [Crossref] [PubMed]
- De Leyn P, Dooms C, Kuzdzal J, et al. Revised ESTS guidelines for preoperative mediastinal lymph node staging for non-small-cell lung cancer. Eur J Cardiothorac Surg 2014;45:787-98. [Crossref] [PubMed]
- Batchelor TJP, Rasburn NJ, Abdelnour-Berchtold E, et al. Guidelines for enhanced recovery after lung surgery: recommendations of the Enhanced Recovery After Surgery (ERAS®) Society and the European Society of Thoracic Surgeons (ESTS). Eur J Cardiothorac Surg 2019;55:91-115. [Crossref] [PubMed]
- Wang C, Lai Y, Li P, et al. Influence of enhanced recovery after surgery (ERAS) on patients receiving lung resection: a retrospective study of 1749 cases. BMC Surg 2021;21:115. [Crossref] [PubMed]
- Drevet G, Ugalde Figueroa P. Uniportal video-assisted thoracoscopic surgery: safety, efficacy and learning curve during the first 250 cases in Quebec, Canada. Ann Cardiothorac Surg 2016;5:100-6. [Crossref] [PubMed]
- Vieira A, Bourdages-Pageau E, Kennedy K, et al. The learning curve on uniportal video-assisted thoracic surgery: An analysis of proficiency. J Thorac Cardiovasc Surg 2020;159:2487-2495.e2. [Crossref] [PubMed]
- Nachira D, Meacci E, Porziella V, et al. Learning curve of uniportal video-assisted lobectomy: analysis of 15-month experience in a single center. J Thorac Dis 2018;10:S3662-9. [Crossref] [PubMed]
- Liu X, Chen X, Shen Y, et al. Learning curve for uniportal video-assisted thoracoscopic surgery lobectomy-results from 120 consecutive patients. J Thorac Dis 2018;10:5100-7. [Crossref] [PubMed]
- Hernandez-Arenas LA, Lin L, Purmessur RD, et al. Uniportal video-assisted thoracoscopic early learning curve for major lung resections in a high volume training center. J Thorac Dis 2018;10:S3670-7. [Crossref] [PubMed]
- Stamenovic D, Messerschmidt A, Schneider T. Cumulative Sum Analysis of the Learning Curve for Uniportal Video-Assisted Thoracoscopic Lobectomy and Lymphadenectomy. J Laparoendosc Adv Surg Tech A 2019;29:914-20. [Crossref] [PubMed]
- Bedetti B, Bertolaccini L, Solli P, et al. Learning curve and established phase for uniportal VATS lobectomies: the Papworth experience. J Thorac Dis 2017;9:138-42. [Crossref] [PubMed]
- Bertolaccini L, Batirel H, Brunelli A, et al. Uniportal video-assisted thoracic surgery lobectomy: a consensus report from the Uniportal VATS Interest Group (UVIG) of the European Society of Thoracic Surgeons (ESTS). Eur J Cardiothorac Surg 2019;56:224-9. [Crossref] [PubMed]
- Yang X, Li M, Yang X, et al. Uniport versus multiport video-assisted thoracoscopic surgery in the perioperative treatment of patients with T1-3N0M0 non-small cell lung cancer: a systematic review and meta-analysis. J Thorac Dis 2018;10:2186-95. [Crossref] [PubMed]
- Hirai K, Takeuchi S, Usuda J. Single-incision thoracoscopic surgery and conventional video-assisted thoracoscopic surgery: a retrospective comparative study of perioperative clinical outcomes†. Eur J Cardiothorac Surg 2016;49:i37-41. [PubMed]
- Dai F, Meng S, Mei L, et al. Single-port video-assisted thoracic surgery in the treatment of non-small cell lung cancer: a propensity-matched comparative analysis. J Thorac Dis 2016;8:2872-8. [Crossref] [PubMed]
- Zhu Y, Liang M, Wu W, et al. Preliminary results of single-port versus triple-port complete thoracoscopic lobectomy for non-small cell lung cancer. Ann Transl Med 2015;3:92. [PubMed]
- Ng CSH, MacDonald JK, Gilbert S, et al. Optimal Approach to Lobectomy for Non-Small Cell Lung Cancer: Systemic Review and Meta-Analysis. Innovations (Phila) 2019;14:90-116. [Crossref] [PubMed]
- Gonzalez CE, Rinaldi MG, Sugar AM. Zygomycosis. Infect Dis Clin North Am 2002;16:895-914. vi. [Crossref] [PubMed]
- Wang L, Liu D, Lu J, et al. The feasibility and advantage of uniportal video-assisted thoracoscopic surgery (VATS) in pulmonary lobectomy. BMC Cancer 2017;17:75. [Crossref] [PubMed]
- Zhao R, Shi Z, Cheng S. Uniport video assisted thoracoscopic surgery (U-VATS) exhibits increased feasibility, non-inferior tolerance, and equal efficiency compared with multiport VATS and open thoracotomy in the elderly non-small cell lung cancer patients at early stage. Medicine (Baltimore) 2019;98:e16137. [Crossref] [PubMed]
- Abouarab AA, Rahouma M, Kamel M, et al. Single Versus Multi-Incisional Video-Assisted Thoracic Surgery: A Systematic Review and Meta-analysis. J Laparoendosc Adv Surg Tech A 2018;28:174-85. [Crossref] [PubMed]
- Yan Y, Huang Q, Han H, et al. Uniportal versus multiportal video-assisted thoracoscopic anatomical resection for NSCLC: a meta-analysis. J Cardiothorac Surg 2020;15:238. [Crossref] [PubMed]
- Louis SG, Gibson WJ, King CL, et al. Uniportal video-assisted thoracoscopic surgery (VATS) technique is associated with decreased narcotic usage over traditional VATS lobectomy. J Vis Surg 2017;3:117. [Crossref] [PubMed]
- Tosi D, Nosotti M, Bonitta G, et al. Uniportal and three-portal video-assisted thoracic surgery lobectomy: analysis of the Italian video-assisted thoracic surgery group database. Interact Cardiovasc Thorac Surg 2019;29:714-21. Erratum in: Interact Cardiovasc Thorac Surg 2019;29:821. [Crossref] [PubMed]
- Harris CG, James RS, Tian DH, et al. Systematic review and meta-analysis of uniportal versus multiportal video-assisted thoracoscopic lobectomy for lung cancer. Ann Cardiothorac Surg 2016;5:76-84. [Crossref] [PubMed]
- Bourdages-Pageau E, Vieira A, Lacasse Y, et al. Outcomes of Uniportal vs Multiportal Video-Assisted Thoracoscopic Lobectomy. Semin Thorac Cardiovasc Surg 2020;32:145-51. [Crossref] [PubMed]
- Perna V, Carvajal AF, Torrecilla JA, et al. Uniportal video-assisted thoracoscopic lobectomy versus other video-assisted thoracoscopic lobectomy techniques: a randomized study. Eur J Cardiothorac Surg 2016;50:411-5. [Crossref] [PubMed]
Cite this article as: Savoie-White FH, Menier CA, Vieira A, Ugalde PA. Uniportal video-assisted thoracoscopic surgery for lung cancer—current practices and outcomes: a narrative review. Curr Chall Thorac Surg 2023;5:40.


