
Patient perspectives on open vs. minimally invasive thoracic surgery (PPOMITS): survey and experience from a single academic institution
Highlight box
Key findings
• Regardless of surgical approach, patients experienced a decline in functional outcomes at 1 month, followed by recovery to baseline at 6 months. Patients placed greater importance on risk of complications following surgery than post-operative pain, incision size, and distance to treatment centre.
What is known and what is new?
• Despite the widespread acceptance of safety and oncologic equivalence of minimally invasive thoracic surgery, adoption by thoracic surgeons is lagging.
• There is limited literature on patient perspectives on minimally invasive thoracic surgery versus open surgical approaches.
What is the implication, and what should change now?
• Patients undergoing cancer resection surgeries may be willing to participate in randomized trials that compare minimally invasive and open surgical approaches.
Introduction
Minimally invasive surgery (MIS) is a surgical technique involving reduced trauma to skin and soft tissue due to smaller incision size. This technique is increasingly being used as the alternative to open surgery for patients eligible for thoracic surgery and includes laparoscopy and video-assisted thoracoscopic surgery (VATS). Once believed to be technically and oncologically superior, open surgery has increasingly fallen out of favour, for both benign and malignant diseases. Two randomized controlled trials (RCTs) have demonstrated a reduction in lung cancer-related morbidity in the first year following VATS compared to a thoracotomy (1,2). Another study found that after 1-year follow-up, patients who received VATS had significantly lower moderate-severe levels of pain and higher self-reported quality of life (QoL) scores relative to those who underwent anterolateral thoracotomy (3). Similar benefits of MIS approaches are seen with esophageal cancer (4). Furthermore, RCTs have demonstrated similar long-term oncological outcomes (5,6), while other evidence supports a shorter length of stay (LOS), less postoperative pain and improved QoL (7-12).
Despite sound evidence supporting minimally invasive approaches in thoracic surgery, acceptance within the surgical community has not been universal (13). Adoption and implementation of minimally invasive thoracic surgery continues to be low with wide variations across countries. MIS accounts for 30–40% of surgeries in North American context (14,15), while in Europe, the rates vary from 29–65% (16-18). Practice variability and a relative lack of uniform approach may in part explain this low uptake. In addition, little is known about patient perspectives regarding the use of MIS compared to open surgical approaches. The challenges of recruiting patients for randomization in surgical trials further adds to the complexity of understanding patient perspectives on surgical procedures (19).
Surgeons may presume a patient-preference for MIS, although to our knowledge this has not been substantiated. The aim of our study was to objectively document patients’ viewpoints on pain, functional outcomes, and treatment expectations following MIS or open surgery, throughout the course of treatment. Involving thoracic surgery patients in RCT-based on patient preferences will elucidate much uncertainty within the field and allow to better address concerns in the thoracic surgery decision-making process. We also examined responses classified by surgical site (neck, chest or abdomen) and geographical distance to treatment centres. We present this article in accordance with the SURGE reporting checklist (available at https://ccts.amegroups.com/article/view/10.21037/ccts-22-10/rc).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Research Ethics Board at the Ottawa Hospital and registered with clinicaltrials.gov (NCT01807390), and informed consent was obtained from all individual participants. Procedures were conducted at a tertiary care academic center consisting of 6 board certified thoracic surgeons. The catchment area extends over 18,000 square kilometers. When patients consent for surgery, they consent to be operated on by any of the six surgeons within the group practice. Patients scheduled for either MIS or open surgeries were approached for participation in the survey. Procedures were determined according to appropriate physician assessment and recommendations. Perioperative work-up, educational material, and postoperative care are standardized through care maps. Patients with pulmonary, mediastinal or esophageal diseases were eligible for the study if they were surgical candidates and over 18 years of age.
Patient demographics, procedural details, and survey-response results were collected prospectively in an encrypted, de-identified database. Participants completed two questionnaires: A pre- and post-operative questionnaire on patient perspectives of open versus minimally invasive thoracic surgery (PPOMITS) (Appendix 1, Appendix 2) and a quality-of-life survey; the RAND 36-item Short Form Health Survey version 1.0 (RAND SF-36) (Appendix 3). Both questionnaires were administered at three time points (preoperatively, 1 month postoperatively, and 6 months postoperatively). Envelopes were provided to patients in order to facilitate returned responses in the postoperative setting.
The PPOMITS questionnaire uses visual analog scales [VAS; 1 (unimportant)–10 (important)] to quantify the relationship between surgical approach (open vs. MIS) and anatomic region of surgery (neck, chest, and abdomen) attempting to understand a patient’s expectations and experiences regarding travel burden, postoperative pain, risk of postoperative complications, cosmesis, and recovery time following the surgical intervention. Questions regarding patient expectations were asked during the pre-operative period, whereas those regarding experienced pain and complications were asked during the post-operative periods. The questions were asked of each anatomic region (neck, chest, and abdomen). The RAND SF-36 comprises 8 domains, aimed at measuring functional outcomes, including: (I) physical functioning; (II) physical pain; (III) role limitations due to physical health problems; (IV) role limitations due to personal or emotional problems; (V) emotional well-being; (VI) social functioning; (VII) energy/fatigue; and (VIII) general health perceptions. Chi-square and Fisher’s exact tests were used for comparison of frequencies between categorical variables of the MIS and open surgery groups in the baseline characteristics table. Independent t-tests were used to assess the difference between the means of continuous variables. These were used to test for statistically significant differences wherever appropriate.
Results
Patient enrollment took place from February 2012 to March 2017. A total of 201 patients participated, with 163 patients in the MIS group and 38 in the open surgery group (Table 1). Patient characteristics within each surgery group are outlined in Table 1. Survey completion rates for the PPOMITS and SF-36 questionnaires are outlined in Table 2. 459 SF-36 and 480 PPOMITS surveys were completed throughout the study. The SF-36 questionnaires included: 180 during the preoperative period, 142 in the 1-month follow up, and 137 during the 6-month follow up period (Table 2).
Table 1
| Baseline characteristics | Incision type | P value | |
|---|---|---|---|
| MIS (n=163) | Open (n=38) | ||
| Age (years), median (SE) | 66 (0.05) | 64 (1.27) | |
| Female sex, n (%) | 103 (63.2) | 16 (42.1) | <0.0001* |
| Diagnosis, n (%) | n=162 | ||
| Esophageal cancer | 6 (3.7) | 3 (7.9) | |
| Lung cancer | 121 (74.2) | 28 (73.7) | |
| Metastasis | 20 (12.3) | 4 (10.5) | |
| Other | 15 (9.2) | 3 (7.9) | |
| Procedure, n (%) | <0.0001* | ||
| Pulmonary wedge | 47 (28.8) | 5 (13.6) | |
| Lobectomy | 95 (58.3) | 21 (55.3) | |
| Pneumonectomy | n/a | 5 (13.2) | |
| Esophagectomy | 6 (3.7) | 4 (10.5) | |
| Other | 15 (9.2) | 3 (7.9) | |
| Post-operative complications, n (%) | n=149 | n=35 | 0.046* |
| Air leaks | 24 (16.1) | 3 (8.6) | |
| Anastomotic leaks | 1 (0.7) | n/a | |
| Cardiac | 10 (6.7) | 5 (14.3) | |
| Pulmonary | 4 (2.7) | 5 (14.3) | |
| Other | 10 (6.7) | 2 (5.7) | |
| None | 100 (67.1) | 20 (57.1) | |
| Epidural use, n (%) | 20 (12.3) | 31 (81.6) | <0.0001* |
*, statistically significant P value, P<0.05. SE, standard error; MIS, minimally invasive surgery; n/a, not applicable.
Table 2
| Questionnaire type | n (%) |
|---|---|
| SF-36 survey (N=201) | |
| Preoperative survey | 180 (89.6) |
| 1-month postoperative survey | 142 (70.6) |
| 6-month postoperative survey | 137 (68.2) |
| PPOMITS questionnaire (N=200) | |
| Preoperative survey | 194 (97.0) |
| 1-month postoperative survey | 147 (73.5) |
| 6-month postoperative survey | 139 (69.5) |
SF-36, 36-item Short Form Health Survey; PPOMITS, patient perspectives on open vs. minimally invasive thoracic surgery.
PPOMITS questionnaire
Experienced pain
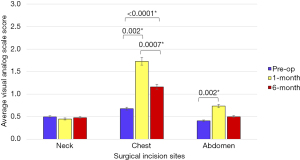
The average score for experienced neck pain did not differ between the three selected time points (preoperative, 1 month postoperative, and 6 months postoperative), however, for both chest and abdominal pain, preoperative pain was lowest followed by a significant increase at 1-month. Although decreased average scores were observed from 1 month postoperatively to 6 months postoperatively, the difference in scores was only significant for chest pain (Figure 1). Mean preoperative pain (0.68; 95% CI: 0.52–0.84) was significantly less than pain experienced postoperatively at 1 month (1.73; 95% CI: 1.41–2.05; P<0.0001) and 6 months (1.16; 95% CI: 0.90–1.42; P=0.002) (Figure 1). Pain experienced after surgery in the chest also significantly decreased going from 1 to 6 months post-operation (P=0.0007). Pain experienced after abdominal surgery was only significantly different between the preoperative time and 1 month post-operation (P=0.002), with lower pain experienced preoperatively (0.41; 95% CI: 0.29–0.52) than postoperatively at 1 month (0.74; 95% CI: 0.48–0.99) (Figure 1).
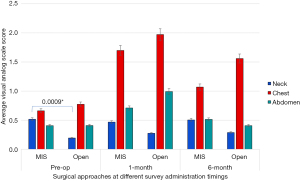
Following stratification, no difference in pain perception was experienced by patients undergoing MIS vs. open surgery, except for those undergoing neck surgery (preoperatively period only) (MIS =0.52; 95% CI: 0.37–0.67; open =0.20; 95% CI: 0.08–0.31; P=0.0009) (Figure 2). No significant difference (P>0.05) in experienced pain was observed in the chest or abdomen at any of the measured times, nor were there are difference in neck pain postoperatively between surgical approaches.
Expectations and perceived concerns regarding pain
When asked to quantify the intensity of post-surgical pain in relationship to incisions in the aforementioned bodily regions, patients had similar expectations whether surgery would be performed in the neck, chest or abdomen (P>0.05). Further, expectations for pain were found to be statistically non-significant between MIS and open approaches regardless of the region of surgical incision or post-op follow-up time (P>0.05) (Figure 3). In addition, concern regarding postoperative pain at both 1 and 6 months was non-significant between MIS and open surgical approaches. Concerns regarding pain were not significantly different between MIS and open approach groups at any point of time for any surgical incision site (P>0.05). Patients in both surgical approach groups had expectations of a high level of pain control at 1-month after the operation regardless of the incision site with values ranging from approximately 7.8–8.5 on the VAS. Similar values were seen for pain control expectations at 6 months following surgery (VAS range, ~7.7–9.0). In the sub-group analysis, there was no significant difference between pain control expectations at 1-month between MIS and open approaches in all three surgical sites (P>0.05). Statistically significant differences between approaches were, however, found for expectations of pain control at 6 months following surgeries to the chest (mean MIS VAS =8.02; 95% CI: 7.69–8.35; mean OPEN VAS =8.75; 95% CI: 8.28–9.22; PMIS vs. open =0.01) and abdominal regions (mean MIS VAS =7.83; 95% CI: 7.41–8.25; mean OPEN VAS =8.96; 95% CI: 8.51–9.41; PMIS vs. OPEN >0.0001).

Expectations regarding risk of complications and daily activities
Expectations for risk of postoperative complications were found to be significantly greater for the open surgical approach (mean VAS =5.73; 95% CI: 4.67–6.78) than MIS (mean VAS =4.53; 95% CI: 4.1–5.0) for chest surgeries, preoperatively (P=0.04). All other evaluated anatomic regions and follow-up times did not significantly differ in patients’ perspectives on expected risk of complications (P>0.05). In both surgical approach groups, across all three time points and all anatomic regions for surgery, patients perceived a moderate risk of complications after surgery, with VAS scores ranging from 4.0 to 5.9.
Both groups felt they would have a moderate-high level of independence with activities of daily living following surgery, with no difference between MIS or an open approach at the 1- or 6-month intervals (P>0.05), ranging from an approximate score of 5.1 to 7.3 on the VAS.
Importance
Overall, patients placed greatest importance on the risk of postoperative complications (mean VAS =7.36; 95% CI: 7.1–7.6) and postoperative pain (mean VAS =6.93; 95% CI: 6.7–7.2). Risk of complications was considered significantly more important than pain (mean difference =0.44; 95% CI: 0.22–0.65; P<0.001) and all other variables, including incision size (mean difference =3.0; 95% CI: 2.69–3.32; P<0.001) and travel burden (mean difference =2.96; 95% CI: 2.6–3.3; P<0.001). Distance to tertiary care centres (mean VAS =4.35; 95% CI: 4.0–4.7) and incision size (mean VAS =4.31; 95% CI: 4.0–4.6) were perceived as less important, respectively, although the difference in importance was not statistically significant (mean difference =0.30; 95% CI: −0.34 to 0.4; P=0.874). Findings for perceived importance, when stratified by time of survey administration relative to the date of surgery, were similar to the overall importance values and across all points of time for most of the pairwise comparisons. Postoperative pain and procedural risk were significantly more concerning to patients than surgical incision size and the distance travelled to obtain the procedure across all three evaluated time points. Comparing the risk of complications and postoperative pain, patients found the former to be of significantly greater importance overall (mean difference =0.44; 95% CI: 0.22–0.65; P<0.001) and at 6 months postoperatively (mean difference =0.76; 95% CI: 0.37–1.14; P<0.001), whereas the difference in mean importance score was not statistically significant when patients were asked preoperatively or at 1-month postoperatively (P>0.05).
In a subgroup analysis, we investigated whether the perceived level of importance differed between patients undergoing MIS vs. open surgery. Findings indicated that the level of importance of any of the evaluated factors (i.e., incision size, distance, postoperative pain, and risk of complications) between groups undergoing either surgical approach did not differ significantly, regardless of surgical incision site and time of survey administration (P>0.05).
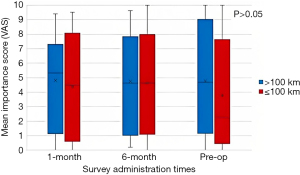
Travel burden
An additional subgroup analysis was conducted classifying patients based on distance from the treating centre (≤100 km from treating centre; >100 km from treating centre), illustrating a wide variability in responses regarding importance of the distance, as an indicator of travel burden at all three points of time (Figure 4). The overall importance of distance to the treatment centres did not differ significantly based on the patients’ actual distance to these centres (P>0.05) at any of the evaluated points of time. The data was then further stratified by anatomic region of surgery. Whether the distance to the treatment centre was >100 or ≤100 km, no significant difference in importance of the distance was observed between MIS and Open groups regardless of anatomic surgical site (P>0.05).
QoL questionnaire
The RAND SF-36 survey completion rates are demonstrated in Table 2. In the 1-month postoperative RAND SF-36 survey, patients perceived the following domains to decrease significantly: physical functioning (P<0.0001), role limitation due to physical health (P<0.0001), social functioning (P<0.0001), energy/fatigue (P<0.0001), and bodily pain (P<0.0001). At the 6-month follow up survey, these five domains of the RAND SF-36 had returned to baseline levels. There was no significant difference in the patient’s perception of emotional well-being, role limitation due to personal or emotional problems, and general health perceptions either at the 1- or 6-month follow up survey [non-significant (NS) result]. The comparison of the change in RAND patient perspective scores from preoperative to 1-month postoperative survey times in MIS vs. open surgical approaches showed no significant differences for all health categories (P>0.05). Similar results were observed between preoperative and 6-month postoperative survey times (Figure 5). We performed a sub-group analysis investigating the effect of open and MIS techniques on the 8 domains of the RAND SF-36 questionnaire. There was no significant difference in the patient’s perception of all 8 QoL domains following either open surgery or MIS, assessed at the 1-month follow-up and at the 6-month follow-up (P>0.05).

Discussion
Our study demonstrates that, regardless of surgical approach, patients regain baseline QoL scores in all domains assessed by the RAND SF-36 at 6 months following their surgery, despite an initial decline in QoL at 1 month. Both MIS and open procedures were well tolerated in terms of physical, emotional, and social domains. Furthermore, results from the PPOMITS questionnaire revealed that patients placed greater importance on postoperative pain and complication risks associated with surgery than on incision size or location (neck, chest, or abdomen), and or travel distance to obtain surgical care. The results of this longitudinal survey challenge the commonly held belief that patients would not accept to be randomized between MIS or open surgery.
Despite RCTs representing the gold standard of clinical research, there is a paucity of well-conducted RCTs comparing MIS to open surgical procedures (20). Some potential reasons include ethical concerns, surgeon attitude, lack of equipoise, low recruitment rates, and patient preference (21). The latter refers to beliefs, expectations, and personal goals, as well as, to the process with which patients balance benefits, harms and inconveniences (22). Patients may be willing to be randomized if their preferences are aligned with the study goals. As an example, from the present study, if patients’ perception of postoperative pain and risk of complications were felt to be identical between surgical approaches, then randomization would likely not be seen as a potential safety concern or a major deviation from standard care.
Our results highlight that patient preferences regarding incision size and travel distance are less important than their concerns about postoperative pain and risk of complications. Due to the invasive nature of surgery and its associated risks, outcomes must be measured to the highest standards of care and best-evidence guidelines. However, guidelines do not always incorporate patient’s input and hence may underestimate/underreport the full range of valued patient outcomes (23). Without identifying patient preferences in RCTs, a source of uncontrolled bias may arise, as the preferences are not dealt with in the randomization process, thus threatening the validity of the outcome (24). As such, patient input should represent an integral aspect of potential surgical RCTs. Despite these drawbacks, patient-oriented, high quality surgical research must remain a priority for our surgical community. Ethical considerations may arise with respect to randomization between MIS and open surgical approaches with mounting non-randomized and randomized evidence suggesting the superiority of minimally invasive surgery for many resectable cancers. If no true clinical equipoise exists, then we would expect a higher dissemination of apparently superior surgical approaches across clinical practice. According to data from major thoracic societies [e.g., Society of Thoracic Surgeons (STS), European Society of Thoracic Surgeons (ESTS)], the percentage of major thoracic surgical procedures being performed using MIS approaches remains limited and largely confined to academic institutions. The lack of randomized data can be a significant obstacle to the development of strong guidelines and to the widespread adoption of newer therapies and procedures. A good example of this would be surgery for colorectal cancer. The MIS approach did not become widely disseminated until a landmark randomized trial showed result in equivalent oncologic outcomes, reduced LOS, improved QoL scores and patient satisfaction (25-28). To our knowledge, there is limited high-level evidence to support MIS over Open surgical treatment of lung or esophageal cancer for example (29,30). The lack of RCTs in surgical research can be partly attributed to surgeon preferences of surgical approach, thereby limiting willingness to participate in this type of study. However, some studies have suggested the possibility of expertise-based RCTs, where surgeons are assigned to a surgical approach for the study period based on their preference and expertise, thus alleviating such concerns (31,32). This represents an opportunity to conduct well-organized studies comparing MIS and open thoracic surgery, helping elucidate whether minimally invasive thoracic surgery can become the new gold standard. Our institutional practice model is that of a single-entry model. Here, single-entry models consist of a centralized intake and coordinated triage approach, assembling patients into a single-queue within a given jurisdiction, allowing more timely and equitable access to care (33).
We acknowledge that our results must be interpreted in light of some limitations. The relatively small sample size in the open surgery group with large range in the confidence intervals lends itself to a type I error, without appropriate power to detect a true difference. More patients undergoing pulmonary resection compared to esophageal resection made up the cohort of respondents. In addition, participants providing their expectations and concerns for MIS were independent of those answering for open surgeries, therefore relative comparisons are subject to bias in the interpretation of the results. Data regarding postoperative pain control was not collected for this study. This is a potential confounding variable for experienced pain at both post-surgical time points. Additionally, we acknowledge that there is no real benefit from an MIS approach in the neck, these cases were included to provide an overall sense of patient perception across all body regions considered in thoracic surgeries. However, it should be noted that this is a potential limitation as no meaningful interventions can be implemented in these cases. Generalizability of the results is also impacted by the fact that this is a single-institution experience. Lastly, the study was subject to selection bias because practices changed over time, including procedure preference. While surgeons who started their career more recently have training in MIS approaches, more senior surgeons tend to have a preference towards open surgeries. Despite these limitations, our primary goal of assessing patient perspectives and subjective responses to a given surgical technique, as well as patient preferences, was still achieved.
Conclusions
Our results demonstrate an initial deterioration in functional outcome, followed by a full recovery by 6 months, regardless of the surgical approach (MIS vs. open) selected. In addition, patients expressed their perception that surgical safety, or the risk of postoperative complications, is a more important concern than incision size, pain, and distance traveled for care when deciding to proceed with surgical therapy for diseases of the chest and upper gastrointestinal tract. Our results suggest that patients may be open-minded to enroll in randomization between open and MIS surgical procedures as long as expectations in regards to postoperative complications and pain management are clearly defined.
Acknowledgments
This research was presented at the IASLC 2018 World Lung Conference in Toronto, Canada (Journal of Thoracic Oncology. 13. S851. 10.1016/j.jtho.2018.08.1525).
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Jean Bussieres and George Rakovich) for the series “Recent Advances in Perioperative Care in Thoracic Surgery and Anesthesia” published in Current Challenges in Thoracic Surgery. The article has undergone external peer review.
Reporting Checklist: The authors have completed the SURGE reporting checklist. Available at https://ccts.amegroups.com/article/view/10.21037/ccts-22-10/rc
Data Sharing Statement: Available at https://ccts.amegroups.com/article/view/10.21037/ccts-22-10/dss
Peer Review File: Available at https://ccts.amegroups.com/article/view/10.21037/ccts-22-10/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at: https://ccts.amegroups.com/article/view/10.21037/ccts-22-10/coif). The series “Recent Advances in Perioperative Care in Thoracic Surgery and Anesthesia” was commissioned by the editorial office without any funding or sponsorship. DEM serves as an unpaid editorial board member of Current Challenges in Thoracic Surgery from December 2021 to November 2023. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Research Ethics Board at the Ottawa Hospital and registered with clinicaltrials.gov (
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lim E, Batchelor T, Dunning J, et al. In hospital clinical efficacy, safety and oncologic outcomes from VIOLET: A UK multi-centre RCT or VATS versus Open lobectomy for lung cancer. J Thorac Oncol 2019;14:S6. [Crossref]
- Bendixen M, Kronborg C, Jørgensen OD, et al. Cost-utility analysis of minimally invasive surgery for lung cancer: a randomized controlled trial. Eur J Cardiothorac Surg 2019;56:754-61. [Crossref] [PubMed]
- Bendixen M, Jørgensen OD, Kronborg C, et al. Postoperative pain and quality of life after lobectomy via video-assisted thoracoscopic surgery or anterolateral thoracotomy for early stage lung cancer: a randomised controlled trial. Lancet Oncol 2016;17:836-44. [Crossref] [PubMed]
- Biere SS, van Berge Henegouwen MI, Maas KW, et al. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet 2012;379:1887-92. [Crossref] [PubMed]
- Situ D, Long H, Tan Q, et al. Video-assisted thoracoscopic surgery vs. thoracotomy for non-small cell lung cancer: survival outcome of a randomized trial. J Thorac Oncol 2019;14:S240. [Crossref]
- van der Sluis PC, van der Horst S, May AM, et al. Robot-assisted minimally invasive thoracolaparoscopic esophagectomy versus open transthoracic esophagectomy for resectable esophageal cancer: a randomized controlled trial. Ann Surg 2019;269:621-30. [Crossref] [PubMed]
- Scott WJ, Allen MS, Darling G, et al. Video-assisted thoracic surgery versus open lobectomy for lung cancer: a secondary analysis of data from the American College of Surgeons Oncology Group Z0030 randomized clinical trial. J Thorac Cardiovasc Surg 2010;139:976-81; discussion 981-3. [Crossref] [PubMed]
- Villamizar NR, Darrabie MD, Burfeind WR, et al. Thoracoscopic lobectomy is associated with lower morbidity compared with thoracotomy. J Thorac Cardiovasc Surg 2009;138:419-25. [Crossref] [PubMed]
- Linden D, Linden K, Oparka J. In patients with resectable non-small-cell lung cancer, is video-assisted thoracoscopic segmentectomy a suitable alternative to thoracotomy and segmentectomy in terms of morbidity and equivalence of resection?. Interact Cardiovasc Thorac Surg 2014;19:107-10. [Crossref] [PubMed]
- Wang H, Shen Y, Feng M, et al. Outcomes, quality of life, and survival after esophagectomy for squamous cell carcinoma: A propensity score-matched comparison of operative approaches. J Thorac Cardiovasc Surg 2015;149:1006-14; discussion 1014-5.e4. [Crossref] [PubMed]
- Higuchi M, Yaginuma H, Yonechi A, et al. Long-term outcomes after video-assisted thoracic surgery (VATS) lobectomy versus lobectomy via open thoracotomy for clinical stage IA non-small cell lung cancer. J Cardiothorac Surg 2014;9:88. [Crossref] [PubMed]
- Luketich JD, Pennathur A, Awais O, et al. Outcomes after minimally invasive esophagectomy: review of over 1000 patients. Ann Surg 2012;256:95-103. [Crossref] [PubMed]
- van Rijswijk AS, Hagens ERC, van der Peet DL, et al. Differences in Esophageal Cancer Surgery in Terms of Surgical Approach and Extent of Lymphadenectomy: Findings of an International Survey. Ann Surg Oncol 2019;26:2063-72. [Crossref] [PubMed]
- Abdelsattar ZM, Allen MS, Shen KR, et al. Variation in Hospital Adoption Rates of Video-Assisted Thoracoscopic Lobectomy for Lung Cancer and the Effect on Outcomes. Ann Thorac Surg 2017;103:454-60. [Crossref] [PubMed]
- Shigemura N, Akashi A, Funaki S, et al. Long-term outcomes after a variety of video-assisted thoracoscopic lobectomy approaches for clinical stage IA lung cancer: a multi-institutional study. J Thorac Cardiovasc Surg 2006;132:507-12. [Crossref] [PubMed]
-
Society of Cardiothoracic Surgery Report - Jakobsen E, Rasmussen TR. The Danish Lung Cancer Registry. Clin Epidemiol 2016;8:537-41. [Crossref] [PubMed]
- ESTS database report. Available online: http://www.ests.org/login.aspx?ReturnUrl=%2fprivate%2fdatabase_reports.aspx
- Chapman SJ, Shelton B, Mahmood H, et al. Discontinuation and non-publication of surgical randomised controlled trials: observational study. BMJ 2014;349:g6870. [Crossref] [PubMed]
- Serrano PE, Bhandari M, Simunovic M. Surgical Culture Shifts and Randomized Clinical Trials. JAMA Netw Open 2021;4:e2115456. [Crossref] [PubMed]
- McLeod RS. Issues in surgical randomized controlled trials. World J Surg 1999;23:1210-4. [Crossref] [PubMed]
- Montori VM, Devereaux PJ, Straus S, et al. Chapter 22.2. Decision making and the patient. In: Guyatt G, Rennie D, Meade MO, et al. editors. Users' Guides to the Medical Literature: A Manual for Evidence-Based Clinical Practice. 2nd ed. Columbus, OH: McGraw-Hill Education, 2008.
- Kunneman M, Marijnen CA, Baas-Thijssen MC, et al. Considering patient values and treatment preferences enhances patient involvement in rectal cancer treatment decision making. Radiother Oncol 2015;117:338-42. [Crossref] [PubMed]
- Brewin CR, Bradley C. Patient preferences and randomised clinical trials. BMJ 1989;299:313-5. [Crossref] [PubMed]
- Bednarski BK, Nickerson TP, You YN, et al. Randomized clinical trial of accelerated enhanced recovery after minimally invasive colorectal cancer surgery (RecoverMI trial). Br J Surg 2019;106:1311-8. [Crossref] [PubMed]
- Lacy AM, Delgado S, Castells A, et al. The long-term results of a randomized clinical trial of laparoscopy-assisted versus open surgery for colon cancer. Ann Surg 2008;248:1-7. [Crossref] [PubMed]
- Colon Cancer Laparoscopic or Open Resection Study Group. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol 2009;10:44-52. [Crossref] [PubMed]
- Ohtani H, Tamamori Y, Arimoto Y, et al. A meta-analysis of the short- and long-term results of randomized controlled trials that compared laparoscopy-assisted and conventional open surgery for colorectal cancer. J Cancer 2011;2:425-34. [Crossref] [PubMed]
- Darling GE, Allen MS, Decker PA, et al. Randomized trial of mediastinal lymph node sampling versus complete lymphadenectomy during pulmonary resection in the patient with N0 or N1 (less than hilar) non-small cell carcinoma: results of the American College of Surgery Oncology Group Z0030 Trial. J Thorac Cardiovasc Surg 2011;141:662-70. [Crossref] [PubMed]
- van Hagen P, Hulshof MC, van Lanschot JJ, et al. Preoperative chemoradiotherapy for esophageal or junctional cancer. N Engl J Med 2012;366:2074-84. [Crossref] [PubMed]
- Cook JA, Campbell MK, Gillies K, et al. Surgeons' and methodologists' perceptions of utilising an expertise-based randomised controlled trial design: a qualitative study. Trials 2018;19:478. [Crossref] [PubMed]
- Devereaux PJ, Bhandari M, Clarke M, et al. Need for expertise based randomised controlled trials. BMJ 2005;330:88. [Crossref] [PubMed]
- Milakovic M, Corrado AM, Tadrous M, et al. Effects of a single-entry intake system on access to outpatient visits to specialist physicians and allied health professionals: a systematic review. CMAJ Open 2021;9:E413-23. [Crossref] [PubMed]
Cite this article as: Jones D, Bhattacharyya U, Yeung C, Martel A, Hanna M, Moledina A, Seely AJE, Maziak DE, Sundaresan SR, Villeneuve PJ, Gilbert S. Patient perspectives on open vs. minimally invasive thoracic surgery (PPOMITS): survey and experience from a single academic institution. Curr Chall Thorac Surg 2023;5:34.


