
Indocyanine green (ICG) fiducial coil guided wedge resection of recurrent adenocarcinoma in a patient with prior segmentectomy: a case report
Highlight box
Key findings
• This case highlights the novel use of the indocyanine green (ICG) dye-soaked fiducial coil technique for a wedge resection of recurrent cancer in a patient with multifocal lung adenocarcinoma with prior right upper lobe apicoposterior segmentectomy.
What is known, and what is new?
• Localizing a pulmonary nodule with an ICG dye-soaked fiducial coil has recently emerged as a promising technique for bronchoscopic lung nodule marking before surgical resection. Previous reports have highlighted the ability to identify the ICG dye-soaked fiducial coil up to several days after deployment.
• The case report described here highlights additional advantages of this localization method in a patient with a recurrence of multifocal adenocarcinoma in the setting of dense adhesions associated with a previous nearby segmentectomy.
What is the implication, and what should change now?
• The ICG dye-soaked fiducial coil has become our preferred method for localizing challenging lung nodules, and we anticipate widespread adaptation of this technique.
Introduction
The widespread utilization of computed tomography (CT) has increased incidental lung nodules (1). In addition, many patients are now eligible for lung cancer screening with annual CT scans to identify lung cancer in its early stages, which frequently manifests by non-solid or part-solid lung nodules (2). Depending on the location and size of the nodule, tissue diagnosis may be obtained by transbronchial biopsy, percutaneous biopsy, or surgical wedge resection. It is acceptable to perform a surgical wedge resection without prior diagnosis, either with the intention for both diagnostic and curative intent or to complete an anatomic resection (segmentectomy or lobectomy) if lung cancer is confirmed in the wedge resection. In the absence of unusual circumstances (fibrothorax, severe emphysema, etc.), it is typically easy to find solid and part-solid nodules larger than 1 cm in diameter located within 1 cm of the visceral pleura. However, smaller, non-solid, deeper nodules or unusual circumstances may benefit from preoperative localization techniques (3). Dye injection for localization can be performed percutaneously under CT guidance or via navigational bronchoscopy. It is usually followed immediately by resection because most dyes dissipate within a few hours (4). The novel technique of utilizing an indocyanine green (ICG) dye-soaked coil builds upon the technique of dye marking. The coil further helps with localization by providing a more enduring marker. This technique, initially developed by Bawaadam et al. (5), had the objective of performing lung nodule marking with delayed surgical resection within 9 days following coil placement. This novel technique has several advantages over previous localization techniques and the possibility of delayed surgical intervention. Since the dye binds firmly to the coil, manipulating the lung parenchyma is not associated with dye dispersion, as is commonly seen when injected without the coil. In addition, the pathologist can identify the coil but not the ICG dye and the coil’s presence can facilitate finding the lesion of interest. Our case report highlights the advantages of using this novel approach in patients with dense adhesions and altered anatomy due to prior lung resection. We present this article in accordance with the CARE reporting checklist (available at https://ccts.amegroups.com/article/view/10.21037/ccts-24-3/rc).
Case presentation
In October 2022, a 76-year-old woman presented with synchronous bilateral upper lobe part-solid nodules. Her initial CT scan demonstrated a 3.1 cm × 2.1 cm part-solid nodule in the right upper lobe and a 2.6 cm part-solid nodule in the left upper lobe. A positron emission tomography (PET)/CT did not show evidence of mediastinal lymphadenopathy or distant metastatic disease. A transbronchial biopsy of the right upper lobe nodule reported atypical cells that were suspicious for malignancy, and a biopsy of the left upper lobe was reported as negative for carcinoma. Despite the biopsy results, the images were suspicious for multifocal adenocarcinoma. Her case was presented at the tumor board, and a recommendation was given to proceed with sequential bilateral upper lobe wedge resections with possible completion segmentectomies. In December 2022, the patient underwent a robotic-assisted right upper lobe wedge resection followed by completion apicoposterior segmentectomy with lymph node dissection. Pathology reported a T1bN0 adenocarcinoma, 60% acinar, 40% lepidic. She was found to have an EGFR mutation. The tumor board recommended adjuvant osimertinib before left upper lobe wedge resection. Starting January 2023, she received osimertinib 80 mg daily. A re-staging chest CT scan in April 2023 demonstrated a decreasing size of the left upper lobe nodule; however, an enlarging part solid nodule located in the superior segment of the right lower lobe. Her case was again presented at the tumor board, and a recommendation was given for right lower lobe wedge resection since decreasing size of left upper lobe nodule suggested a good response to osimertinib, while increasing size of the right lower lobe nodule could represent resistance and concern for more rapid progression. Axial CT chest showed a ground glass opacity (2.4 cm) with a nodular component (1 cm) in the superior segment of the right lower lobe (Figure 1A). Given the anticipated adhesions and distorted anatomy from previous surgery, ion robotic navigational bronchoscopy was performed by interventional pulmonology for localization of the suspicious lesion in the operating room immediately before lung resection in May 2023. A fiducial coil (6 mm × 3 mm tapering diameter, 5.8 cm extended length; Cook Tornado Coil, Cook Medical, Bloomington, IN, USA) was soaked with 0.25 mL of 2.5 mg/mL concentration ICG dye for 10 minutes of dwell time. The ICG dye-impregnated fiducial coil was loaded in a 1.8 mm outer diameter catheter and deployed into the target area by robotic navigational bronchoscopy under fluoroscopic guidance with Ion endoluminal system (Figure 1B). This was immediately followed by robotic surgery for a wedge resection of the superior segment of the right lower lobe. No side effects or adverse events were associated with the placement of the ICG-impregnated coil.
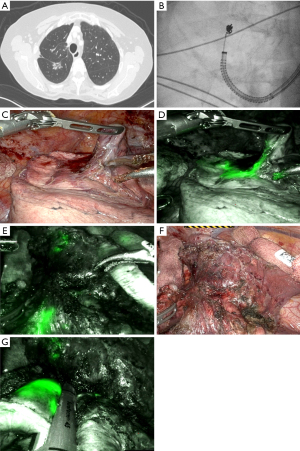
Dense adhesions were encountered, particularly between the remaining anterior segment of the right upper lobe and the right lower lobe superior segment (Figure 1C). The firefly fluorescence imaging system of the da Vinci robotic platform was utilized to visualize the ICG dye-soaked fiducial coil (Figure 1D). The exact localization of the lesion by the ICG dye-soaked fiducial coil was essential to guide the dissection of adhesions (Figure 1E,1F) and perform a wedge resection with negative margins (Figure 1G). X-ray of the surgical specimen revealed the coil within the nodule (Figure 2A,2B). The pathology lab dissected the surgical specimen to locate the target nodule next to the coil.
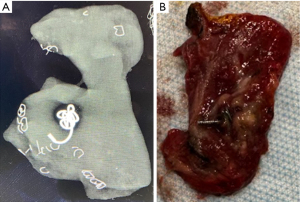
Pathology of the nodule reported the presence of adenocarcinoma with lepidic pattern. A completion right lower lobe superior segmentectomy with lymph node dissection was performed. Final pathology reported minimally invasive adenocarcinoma, lepidic 60%, acinar 40%. She had no postoperative complications. She recovered well and was restarted on adjuvant osimertinib 80 mg daily in June 2023. In September 2023, she underwent robotic-assisted thoracoscopic left upper lobe wedge resection followed by completion left upper lobe apicoposterior segmentectomy with lymph node dissection. Pathology reported ypT1aN0 residual adenocarcinoma spanning 40% of the tumor bed. She had no postoperative complications. She recovered well and continued osimertinib 80 mg daily with a planned treatment duration of 3 years. A surveillance chest CT scan was performed in April 2024, and no evidence of recurrence was reported. She is scheduled for a surveillance chest CT scan every 6 months until September 2026 and yearly after that.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
In addition to the increasing adoption of low-dose chest CT scans for lung cancer screening, the widespread use of CT scans has resulted in a large number of incidentally found lung nodules. Survival after lung cancer surgery is inversely related to the size of the tumor. Five-year survival for a tumor smaller than 10 mm is 92%, while only 83% for tumors 10 to 20 mm (4). To provide patients with the best probability of survival, a lung wedge resection could be offered as a simultaneous diagnostic and therapeutic option for lung nodules suspicious of lung cancer. However, wedge resection as an initial diagnostic modality is usually limited to solid nodules larger than the distance from the nodule to the visceral pleura (6). Several methods have been utilized to locate nodules that do not meet such criteria, including non-solid nodules and sub-centimeter solid or part-solid nodules 1 cm farther from the visceral pleura (7). Wire localization has been described; however, it requires a hybrid operating room (OR) with a chest CT scan, and it may be associated with pneumothorax, hemothorax, and dislodging of the wire before wedge resection (8). Dye marking with ICG and methylene blue has also been described as percutaneous or transbronchial. Bronchoscopic dye injection has been associated with less risk of pneumothorax and hemothorax than CT-guided percutaneous dye injection techniques (9). A disadvantage of the bronchoscopic technique is potential spillage inside the airway or the pleural cavity if the visceral pleura is punctured, resulting in inaccurate marking (10). Nodule localization using fiducials typically requires fluoroscopy during wedge resection.
Localizing a pulmonary nodule with an ICG dye-soaked fiducial coil was initially developed by Bawaadam et al. as a novel approach for bronchoscopic lung nodule marking with delayed surgical resection within 9 days following coil placement (5). The novel technique of utilizing an ICG dye-soaked coil builds upon the technique of dye marking. The coil further helps with localization by providing a more enduring marker, particularly with nodules that are difficult to palpate (5). It also allows for delayed wedge resection, which is helpful if thoracic surgery is not immediately available (4,11).
Furthermore, in contrast to isolated dye markings that cannot be identified in the gross specimen to direct pathologic sectioning, a coil can guide the pathologist during a frozen section, particularly in small non-solid nodules. Our case report highlights the advantage of using this novel approach in a patient with altered anatomy due to prior right upper lobe segmentectomy and significant adhesions. There is a synergistic advantage of combining fiducial and dye marking. Accurate localization of the nodule with prior marking avoided the high probability of a non-diagnostic wedge resection. A coil without ICG-soaking would have been indistinguishable from the nodularity associated with the inflammatory reaction to her prior operation. Isolated ICG dye marking without the coil would have been dispersed during dissection with the inability to guide precise margins for the wedge resection.
The high cost of using the ion robotic bronchoscope could be a limiting factor for this approach. A skilled Interventional Pulmonologist is also required. Without real-time cone beam CT availability, CT divergence could hinder successful targeting. The fact that the entire procedure could be done under a single anesthesia session was convenient for the patient.
Conclusions
In summary, our case report highlights the advantage of using robotic bronchoscopy placement of ICG-impregnated fiducial coil for nodule localization in a patient with dense adhesions and altered anatomy due to prior lung resection. There is a synergistic advantage of combining fiducial and dye marking that facilitates the identification of pulmonary lesions by surgeons and pathologists in challenging scenarios.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://ccts.amegroups.com/article/view/10.21037/ccts-24-3/rc
Peer Review File: Available at https://ccts.amegroups.com/article/view/10.21037/ccts-24-3/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ccts.amegroups.com/article/view/10.21037/ccts-24-3/coif). N.V. received Ziosoft paid for the AATS meeting in Los Angeles in May 2023 registration, flight ticket, and hotel. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hendrix W, Rutten M, Hendrix N, et al. Trends in the incidence of pulmonary nodules in chest computed tomography: 10-year results from two Dutch hospitals. Eur Radiol 2023;33:8279-88. [Crossref] [PubMed]
- Henschke CI, Yankelevitz DF, Mirtcheva R, et al. CT screening for lung cancer: frequency and significance of part-solid and nonsolid nodules. AJR Am J Roentgenol 2002;178:1053-7. [Crossref] [PubMed]
- Jiang J, Lv FJ, Tao Y, et al. Differentiation of pulmonary solid nodules attached to the pleura detected by thin-section CT. Insights Imaging 2023;14:146. [Crossref] [PubMed]
- Gex G, Pralong JA, Combescure C, et al. Diagnostic yield and safety of electromagnetic navigation bronchoscopy for lung nodules: a systematic review and meta-analysis. Respiration 2014;87:165-76. [Crossref] [PubMed]
- Bawaadam H, Benn BS, Colwell EM, et al. Lung Nodule Marking With ICG Dye-Soaked Coil Facilitates Localization and Delayed Surgical Resection. Ann Thorac Surg Short Rep 2023;1:221-5. [Crossref]
- Iqbal SI, Molgaard C, Williamson C, et al. Purposeful creation of a pneumothorax and chest tube placement to facilitate CT-guided coil localization of lung nodules before video-assisted thoracoscopic surgical wedge resection. J Vasc Interv Radiol 2014;25:1133-8. [Crossref] [PubMed]
- Zhang C, Lin H, Fu R, et al. Application of indocyanine green fluorescence for precision sublobar resection. Thorac Cancer 2019;10:624-30. [Crossref] [PubMed]
- Imperatori A, Nardecchia E, Cattoni M, et al. Perioperative identifications of non-palpable pulmonary nodules: a narrative review. J Thorac Dis 2021;13:2524-31. [Crossref] [PubMed]
- Wang L, He J, Zhang L, et al. A novel preoperative image-guided localization for small pulmonary nodule resection using a claw-suture device. Sci Rep 2023;13:18950. [Crossref] [PubMed]
- Ashraf SF, Lau KKW. Navigation bronchoscopy: A new tool for pulmonary infections. Med Mycol 2019;57:S287-93. [Crossref] [PubMed]
- Suzuki K, Nagai K, Yoshida J, et al. Video-assisted thoracoscopic surgery for small indeterminate pulmonary nodules: indications for preoperative marking. Chest 1999;115:563-8. [Crossref] [PubMed]
Cite this article as: Padbidri V, Huang A, Chow N, Arias S, Villamizar N. Indocyanine green (ICG) fiducial coil guided wedge resection of recurrent adenocarcinoma in a patient with prior segmentectomy: a case report. Curr Chall Thorac Surg 2024;6:19.


