
The role of extended reality in enhancing surgical training: a narrative review
Introduction
With the evolving landscape of healthcare systems globally, there is growing demand for surgical training outside the operating room. The 2003 Accreditation Council for Graduate Medical Education (ACGME) regulations in the United States reduced work hours for surgical trainees, requiring them to achieve proficiency in less time (1). Coupled with the high cost of operating room space and declining reimbursements, this has pressured surgical training programs to move beyond the traditional apprenticeship model (2). Additionally, an increased focus on patient safety has necessitated training strategies that do not involve live patients, leading to the expanded use of simulators in surgical education (2). Despite these changes, trainees have become more likely to seek out fellowship training opportunities to obtain more surgical practice (3). However, trainees are also graduating with lower confidence levels in their own ability to operate (4,5). There is a critical need to develop better simulation models that can help improve the technical skills for novice surgeons.
A simulator is a tool or model designed to train individuals by replicating real-life scenarios they will encounter. Training simulators can be considered “low fidelity” or “high fidelity”, depending on the realism of the simulation (6). Low fidelity simulators can be used to practice skills like knot tying or simple sutures on a skin model (7). High fidelity models are more critical in advanced operations or components of operations, like cardiopulmonary bypass, which requires a greater level of realism to help teach the trainee how to operate on a beating heart with potential catastrophic bleeding (8,9). High fidelity simulators include human cadavers, live animals, bench-top models, and extended reality (XR) systems to recreate specific surgical situations, allowing trainees to practice and refine their skills (10).
With simulators, trainees can repeatedly perform techniques and manage complications in a risk-free environment until they achieve proficiency. One challenge or limitation with most current simulation curricula is the need for an educator to help guide the trainee through the steps (11). This educator, likely a surgeon, is needed to instruct trainees initially, but also provide corrective directions on techniques during the practice sessions. The time spent by trained surgeons are currently not re-imbursed, and may take time away from their ability to perform operations that provide the financial support for their program (12).
The integration of XR technologies has the potential to revolutionize healthcare training. XR, including virtual reality (VR) and augmented/mixed reality (AR/MR), offers sophisticated yet accessible simulations that enhance both technical and nontechnical skills among healthcare professionals. Research indicates that XR-based procedural training significantly improves accuracy and quality, especially in novice trainees, by narrowing the performance gap between beginners and experts (13). In addition, XR simulations have been proven to reduce clinical errors and improve outcomes, highlighting the transformative potential of XR in medical education and training (14).
This narrative review provides an updated synthesis of recent advancements in XR technology for surgical education, incorporating the latest developments in AI integration, haptic feedback, and XR applications. While previous literature has examined XR’s general role in surgical training, this review emphasizes its impact on cardiothoracic surgery (CTS), particularly in complex procedures such as cardiac bypass, valve repair, and thoracic interventions. Furthermore, it explores the limitations of XR in cardiothoracic surgical education, including challenges in replicating intricate cardiac anatomy and hemodynamic variability. By evaluating current technologies and methodologies, this review highlights future directions and the potential of XR-driven simulation in advancing cardiothoracic surgical training. We present this article in accordance with the Narrative Review reporting checklist (available at https://ccts.amegroups.com/article/view/10.21037/ccts-24-43/rc).
Methods
This narrative review aims to explore the role of XR in surgical education, with a specific focus on applications in CTS. While this is not a systematic or scoping review, a structured approach was implemented to the literature selection and synthesis to ensure clarity and transparency (Table 1).
Table 1
| Items | Specification |
|---|---|
| Date of search | August–October, 2024 |
| Databases and other sources searched | PubMed, Google Scholar |
| Search terms used | “Extended reality in surgical education” OR “cardiothoracic surgery simulation” |
| Timeframe | Jan 01, 2000–Jul 01, 2024 |
| Inclusion criteria | Peer-reviewed and review articles that discussed the use of XR technologies in surgical education, focused on VR, AR, MR, or hybrid simulation models or provided insights into CTS training |
| Selection process | Conducted independently by one reviewer (J.B.), who screened titles and abstracts for relevance. Full-text articles were then reviewed for inclusion. In cases of ambiguity or uncertainty, a consensus was reached through discussion with additional team members |
AR, augmented reality; CTS, cardiothoracic surgery; MR, mixed reality; VR, virtual reality; XR, extended reality.
A comprehensive search of the literature was conducted to identify studies published between 2000 and 2024 on XR technologies in surgical education, focusing on VR, AR, MR, and simulation in surgical training, particularly in CTS. The search included peer-reviewed articles and review papers from databases such as PubMed and Google Scholar. Key search terms included “extended reality in surgical education”, OR “cardiothoracic surgery simulation”.
Studies were included if they discussed the use of XR technologies in surgical education, focused on VR, AR, MR, or hybrid simulation models or provided insights into CTS training. The selection process was conducted independently by one reviewer, who screened titles and abstracts for relevance. Full-text articles were then reviewed for inclusion. In cases of ambiguity or uncertainty, a consensus was reached through discussion with additional team members. The findings were then synthesized to provide a comprehensive discussion on the current landscape, benefits, limitations, and future directions of XR in CTS training.
Evolution of surgical simulation
Surgical simulation has evolved significantly over the past few decades, transforming from basic models and cadaver-based systems to include sophisticated virtual environments. One of the earliest recorded examples comes from India around 600 B.C., where leaf and clay models were used to conceptualize nasal reconstruction with a forehead flap (15). Historically, training relied heavily on wooden bench top models, live animals, and human cadavers, to practice new techniques, offering limited opportunities for repeated practice and posing ethical concerns (16). Prior to 2003, there was less of a focus on the use of surgical simulation in training programs, when trainees were routinely working more than 100 hours per week.
The advent of computerized simulators in the late 20th century marked a pivotal shift in simulation training (Figure 1). The first commercially successful manikins, known as the Comprehensive Anesthesia Simulation Environment, were designed to train and assess physicians in anesthesia and critical care (17). These early models utilized microprocessor chips and software to simulate vital signs that responded to medical interventions and emergencies (17). Since then, mannequins have evolved, incorporating wireless technologies, high-fidelity human likeness, and advanced computer imaging to enable remarkably realistic training for a wide range of surgical procedures (18).
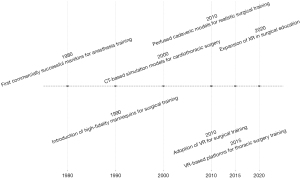
As technology advanced, so did the complexity and realism of surgical simulators. The most significant breakthrough came with the introduction of computed tomography (CT)-based simulation models, particularly in CTS, where precise anatomical detail is critical (19,20). Perfused cadaveric models now provide a realistic training experience by maintaining vascular flow and tissue consistency, closely mimicking live surgical conditions. These models have been instrumental in training cardiothoracic surgeons in complex procedures such as, coronary artery bypass grafting, valve replacements, and thoracic aortic repairs (21). Perfused cadaveric models allow surgeons to practice techniques in a realistic physiological setting, enhancing their ability to manage intraoperative bleeding and tissue manipulation.
Additionally, XR-based simulation models have enabled cardiothoracic surgeons to refine their skills in video-assisted thoracoscopic surgery and robotic-assisted thoracic surgery. XR-based platforms utilize patient-specific CT-derived three-dimensional (3D) reconstructions, allowing trainees to interact with anatomically accurate models in a controlled, risk-free environment (22-24).
Over time, XR simulators have combined realistic computerized images with actual surgical tools, creating high-fidelity AR or MR training experiences (25-27). Today, advancements in computing power, graphics, and haptic feedback have transformed XR-based training into an indispensable tool for CT education. Modern XR platforms now allow for real-time manipulation of CT-derived anatomical models, perfused tissue simulation, and collaborative remote training.
XR enhancing surgical competence
Recent literature underscores the growing integration of XR technologies across diverse surgical specialties, including orthopedic surgery, neurosurgery, and minimally invasive procedures like laparoscopy (25,28). These advancements not only enhance surgical practice but also pave the way for significant improvements in training and education. By leveraging both AR and VR, surgical teams are finding innovative ways to improve outcomes, enhance precision, and refine the skills of surgeons at all levels.
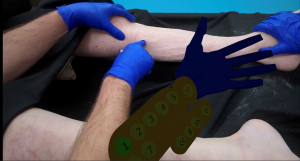
AR has emerged as a powerful option in the surgical toolkit, overlaying digital information onto the surgeon’s real-world view. This technology assists in preoperative planning and intraoperative navigation, facilitating a more informed approach to complex procedures. For instance, it has demonstrated superior accuracy in identifying anatomical variations among patients—variations that may not be evident in conventional imaging methods such as CT scans (29,30). This capability enhances spatial awareness, allowing surgeons to visualize critical structures and align instruments accurately. The ability to see digital overlays in real time contributes to improved decision-making and can significantly reduce the risk of complications. AR in the simulation space may allow for better learning for the novice trainee. The overlap with traditional simulators (like a mannequin), allows the trainees to benefit from the haptic feedback of solid materials during a simulation (31) (Figure 2).
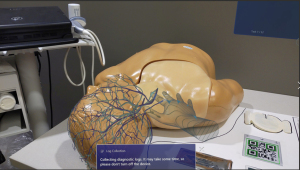
In contrast, VR offers an immersive, fully simulated environment where surgeons can engage in a wide range of procedures (Figure 3). Research has demonstrated that VR enhances procedural accuracy, skill retention, and trainee confidence compared to training using a surgical video (32). VR can play a pivotal role in the pre-operative reconstruction of complex structures, significantly aiding surgeons in visualizing and understanding vascular anatomy, which is crucial for safe vessel control during surgery (33). Additionally, immersive VR systems can enhance surgeons’ understanding of critical anatomical structures, particularly those key sites that are difficult to visualize directly. For instance, studies have shown that VR technology improves the localization of lesions that require resection, which may be obscured from direct view during surgery (34,35). This advancement leads to multiple benefits, including reduced operative time, minimized damage to surrounding tissues, decreased blood loss, and shorter hospital stays for patients (34,35).
XR technologies are playing an increasingly important role in CTS. XR is being leveraged in preoperative planning, intraoperative navigation, and advanced anatomical visualization, offering surgeons a multi-dimensional, patient-specific view of complex structures (Figure 4). One of the most promising applications is in robotic-assisted thoracic surgery training, where XR platforms enable surgeons to simulate robotic procedures in a risk-free environment before performing them in real-life settings (36). Furthermore, patient-specific 3D modeling allows for a personalized surgical strategy, helping surgeons analyze anatomical variations, predict challenges, and optimize their approach for better clinical outcomes (23).

Another groundbreaking advancement is virtual mentorship and remote surgical education through XR (37,38). With XR-driven platforms, experienced cardiothoracic surgeons can potentially provide real-time guidance and supervision to trainees across different geographic locations, fostering global knowledge exchange and collaboration. This is particularly beneficial in regions with limited access to specialized CTS training, as it enables remote learning, case discussion, and procedural demonstrations in an immersive, interactive environment. By integrating these capabilities, XR is not only enhancing surgical education but also bridging the gap in global surgical training accessibility.
The adaptability of XR technologies across various stages of surgical education—from early skill acquisition to the refinement of advanced techniques—positions them as promising adjuncts to conventional apprenticeship models. By incorporating these innovative tools into surgical training programs, educators can create more engaging and effective learning experiences. This shift not only prepares residents for the challenges they will face in the operating room but also fosters a culture of continuous learning and improvement in surgical practice.
XR practice at our institution
Briefly, our institution has developed an XR Central Line Insertion procedural training application. Developed within Unity, it provides audio and visual feedback to the learner through pictures, video tutorials, 3D objects including anatomic overlays, gesture elements, 3D animations, and a step-by-step procedural workflow aligned with proper central line insertion technique and focusing on critical elements of the procedure (Figure 5). The trainer aims to reduce potential patient complications while providing speed and efficiency in completion of the procedure by the trainee. This should reduce the need for faculty time proctoring these simulations. Early prototype testing by colleagues in our nursing school have shown benefit in terms of usability, feasibility, and engagement while also providing a noninferiority to traditional training methods with a maintenance of 100% competency scores and a reduction in faculty time and effort by 75%.
The model is still in the early stages of development and has not yet been formally adopted across our institution due to technological and implementation constraints. While preliminary data suggest promising benefits, further research is required to establish long-term efficacy and feasibility in broader surgical training applications. Additionally, prior research from our group has explored Microsoft HoloLens 2 and Microsoft Guides as XR training tools. However, the discontinuation of these platforms poses challenges for sustained scalability and long-term usability. In response, we are transitioning to a Unity-based development framework that is hardware-agnostic, allowing for greater adaptability across various mixed-reality headsets and platforms. This strategic shift aims to ensure long-term accessibility, scalability, and sustainability for future XR-based surgical training applications.
At this stage, institution-wide studies have not yet been conducted to assess the direct impact of the model on surgical training. However, ongoing research is focused on enhancing the technology and conducting validation studies to evaluate its effectiveness in real-world surgical education environments. Additionally, future directions include expanding the platform to simulate complex bedside procedures, such as extracorporeal membrane oxygenation cannulation and integrating volumetric capture technology to assess procedural sterility and adherence to surgical protocols (39).
Limitations of XR in surgical simulation
While XR technologies offer significant advantages in surgical training, their integration into medical education presents several challenges, including cost, accessibility, and technological limitations. One major concern is the reliability and realism of XR-based simulations (40). Critics argue that, despite advancements, XR systems cannot fully replicate the unpredictability and complexity of real-life surgeries (41). For instance, while VR provides detailed three-dimensional models, most interfaces rely on handheld controllers that do not support the execution of technical skills (42). Laparoscopic trainers are an exception (31). However, VR simulations often lack haptic feedback and the ability to detect fine hand movements, which are essential for replicating real-world surgical procedures (31). This limitation raises concerns that over-reliance on XR training may leave trainees underprepared for the challenges of live surgery, particularly in high-stakes environments. As such, VR solutions may be best used for experienced surgeons who need a “refresher” in content or to be shown examples of new techniques, but do not necessarily need the same hands-on component as a novice trainee would.
A particularly relevant challenge in cardiothoracic surgical education is the difficulty in replicating intricate cardiac anatomy and hemodynamic variability within XR-based simulations (43,44). CTS require precise coordination of multiple surgical and physiological factors, including real-time cardiac motion, blood flow dynamics, and the interaction of surgical instruments with delicate tissues. Current XR technologies struggle to accurately model these complexities, limiting their ability to fully replace traditional hands-on training methods. Additionally, the simulation of cardiopulmonary bypass, valve repair, and coronary interventions remains a major hurdle due to the need for highly realistic hemodynamic responses and tissue mechanics. These limitations highlight the need for advanced computational modeling and real-time physiological integration to enhance the fidelity of XR-based cardiothoracic training platforms.
To address the challenge of limited haptic feedback, emerging technologies such as force-feedback gloves, soft robotics, and electrotactile stimulation are being explored to enhance the tactile realism of XR-based simulations. Force-feedback gloves can replicate resistance and force sensations, improving the realism of surgical interactions, while soft robotic interfaces can provide more nuanced pressure responses to mimic tissue manipulation (45,46). Integrating these technologies into XR platforms has the potential to bridge the gap between virtual simulations and hands-on surgical experience.
Another concern is the significant cost associated with the hardware and software coding and accessibility of XR technologies (41). While large medical centers with significant resources may be able to afford sophisticated XR setups, smaller institutions or those in developing regions may not have access to these tools. This could exacerbate existing inequalities in surgical training and education, as only trainees in well-funded institutions may benefit from these cutting-edge technologies. The initial investment in XR hardware, software, and maintenance, combined with the necessary time to familiarize users with the technology, presents a significant barrier to its universal integration into surgical education.
In response to cost concerns, a shift toward hardware-agnostic XR platforms is emerging. These platforms are designed to be compatible with a range of devices, including lower-cost headsets, laptops, and even mobile devices, reducing reliance on expensive proprietary systems. Additionally, the development of open-source XR software solutions have the potential to lower costs significantly, enabling institutions to customize their own training modules without the constraints of costly licensing fees (47,48). These advancements could democratize access to XR-based training, making it feasible for a broader range of institutions.
Beyond financial constraints, XR implementation faces additional challenges in global settings, particularly in resource-limited regions. High-income countries have greater access to robust technological infrastructure, but in many parts of the world, limited internet bandwidth and unreliable power supply hinder the full integration of cloud-based XR applications and remote mentorship programs (38). Many institutions in developing regions also lack the physical space and infrastructure required to house dedicated XR simulation centers. These barriers make widespread adoption difficult and highlight the need for cost-effective XR solutions that can function in low-resource environments.
One potential solution to improve accessibility is the development of cloud-based XR platforms that allow users to participate in simulations remotely while accounting for infrastructure limitations. By optimizing XR simulations for low-bandwidth environments and leveraging adaptive streaming technologies, cloud-based platforms can minimize the computational burden on individual devices without requiring high-end local hardware. Additionally, hybrid solutions that combine offline XR modules with periodic cloud updates could enhance accessibility in regions with inconsistent internet access. This approach would enable surgical trainees from various locations to engage in immersive training experiences without requiring expensive equipment while ensuring feasibility in low-resource settings.
Finally, it has been shown that XR can increase surgeon confidence, this also raises concern whether XR could inadvertently lead to overconfidence among trainees (49-51). While XR provides a risk-free environment to practice procedures, the lack of real-world consequences in virtual simulations may lead some trainees to underestimate the gravity of certain decisions when they perform actual surgeries. Without the real-life pressure of patient outcomes at stake, there is concern that the safety net of XR training may foster a false sense of security, which could impact decision-making in real operations.
Given the rapidly evolving nature of XR technologies in surgical education, institutions should prioritize solutions that enhance accessibility, scalability, and long-term sustainability. A key approach is the transition to hardware-agnostic platforms that minimize reliance on proprietary devices, ensuring broader adoption and adaptability. The recent discontinuation of platforms like the HoloLens2 and Magic Leap, alongside the rise of newer devices such as the Quest 3 and Apple Vision Pro, underscores the necessity of flexible, software-driven training methodologies. Future research should focus on validating these adaptable frameworks to ensure that XR technologies effectively supplement or replace traditional surgical training while remaining resilient to ongoing technological advancements.
Future directions
As XR technology evolves, its role in surgical training is expected to expand beyond instruction into skill assessment. These platforms could revolutionize competency-based education by providing objective evaluations of procedural accuracy, decision-making, and technical proficiency. Future research should explore the integration of XR into standardized assessments, leveraging real-time data analytics to enhance feedback and personalized training.
As XR technologies continue to advance, their role in surgical training is likely to expand, offering even more sophisticated simulations and personalized learning environments. Currently, XR has demonstrated its ability to replicate some complex surgical procedures in a controlled, immersive setting. However, future developments will likely go beyond simply replicating reality. Emerging technologies, such as artificial intelligence (AI), could be integrated into these systems, resulting in dynamic, adaptive simulations that adjust to the individual skill level of each surgeon. AI-driven XR systems might offer personalized scenarios that evolve based on real-time performance, helping trainees refine their techniques by responding to their specific strengths and weaknesses. For example, an AI-enabled XR system could increase the complexity of a procedure if the user consistently performs well, give instant feedback to the learner, test for competency based on an accepted rubric, or suggest additional practice for areas where they struggle (52).
In CTS, real-time physiological integration and computational modeling will be essential for improving simulation fidelity. Current XR-based CTS training platforms struggle to replicate intricate cardiac anatomy, hemodynamic variability, and the delicate interaction of surgical instruments with dynamic cardiovascular structures. Future research should prioritize the development of high-fidelity physiological modeling, including realistic cardiopulmonary bypass simulations, valve repair techniques, and coronary interventions. The incorporation of biomechanical feedback systems could further improve the accuracy of procedural training in high-risk cardiothoracic surgeries.
Overall, the integration of XR into surgical training marks a paradigm shift in both how surgeons are educated and how they approach their clinical practice. Traditional surgical training, while effective, often follows a standard model where trainees progress through predefined stages of learning regardless of their individual learning pace. With AI-enhanced XR simulations, this rigidity would give way to a more fluid, personalized approach, allowing surgeons to train at their own pace and focus on the areas where they need the most improvement. This individualized training could significantly accelerate skill acquisition and proficiency, enabling surgeons to reach competency faster and with greater confidence.
XR’s potential for collaboration and remote learning could also reshape surgical education globally (53). With the ability to create shared virtual environments, surgeons and trainees from across the world could participate in the same training exercises or surgeries without being physically present in the same room. This opens up possibilities for international collaboration, knowledge exchange, and collective learning, all of which could help elevate the standard of surgical care worldwide.
Conclusions
The future of surgery is increasingly digital, and XR technologies are at the forefront of this transformation. As these technologies become more widely adopted, ongoing research and development will be crucial to fully realize their potential. This includes fine-tuning the accuracy and realism of simulations, addressing cost and accessibility challenges, and ensuring that XR-based training complements hands-on experience in real-life surgical settings.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://ccts.amegroups.com/article/view/10.21037/ccts-24-43/rc
Peer Review File: Available at https://ccts.amegroups.com/article/view/10.21037/ccts-24-43/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://ccts.amegroups.com/article/view/10.21037/ccts-24-43/coif). R.M.R.’s institution received grants from Atricure and On Target Labs. His institution also received consulting fees from Trinity Health and Intuitive Surgical. R.M.R. received payment from BMA. He is also a board member of Genentech, Astra Zeneca, and Metronic. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Philibert I, Friedmann P, Williams WT, et al. New requirements for resident duty hours. JAMA 2002;288:1112-4. [Crossref] [PubMed]
- Ziv Stephen D Small Paul Root Wolpe A. Patient safety and simulation-based medical education. Med Teach 2000;22:489-95. [Crossref]
- Fitzgerald JE, Milburn JA, Khera G, et al. Clinical fellowships in surgical training: analysis of a national pan-specialty workforce survey. World J Surg 2013;37:945-52. [Crossref] [PubMed]
- Coleman JJ, Esposito TJ, Rozycki GS, et al. Early subspecialization and perceived competence in surgical training: are residents ready? J Am Coll Surg 2013;216:764-71; discussion 771-3. [Crossref] [PubMed]
- Fonseca AL, Reddy V, Longo WE, et al. Operative confidence of graduating surgery residents: a training challenge in a changing environment. Am J Surg 2014;207:797-805. [Crossref] [PubMed]
- Massoth C, Röder H, Ohlenburg H, et al. High-fidelity is not superior to low-fidelity simulation but leads to overconfidence in medical students. BMC Med Educ 2019;19:29. [Crossref] [PubMed]
- Williams TP, Snyder CL, Hancock KJ, et al. Development of a Low-cost, High-fidelity Skin Model for Suturing. J Surg Res 2020;256:618-22. [Crossref] [PubMed]
- Hermsen JL, Mohamadipanah H, Yang S, et al. Multimodal Cardiopulmonary Bypass Skills Assessment Within a High-Fidelity Simulation Environment. Ann Thorac Surg 2021;112:652-60. [Crossref] [PubMed]
- Feins RH, Burkhart HM, Conte JV, et al. Simulation-Based Training in Cardiac Surgery. Ann Thorac Surg 2017;103:312-21. [Crossref] [PubMed]
- Cardoso SA, Suyambu J, Iqbal J, et al. Exploring the Role of Simulation Training in Improving Surgical Skills Among Residents: A Narrative Review. Cureus 2023;15:e44654. [Crossref] [PubMed]
- Elendu C, Amaechi DC, Okatta AU, et al. The impact of simulation-based training in medical education: A review. Medicine (Baltimore) 2024;103:e38813. [Crossref] [PubMed]
- Shea S, Nickerson KG, Tenenbaum J, et al. Compensation to a department of medicine and its faculty members for the teaching of medical students and house staff. N Engl J Med 1996;334:162-7. [Crossref] [PubMed]
- Stanney KM, Archer J, Skinner A, Horner C, Hughes C, Brawand NP, et al. Performance gains from adaptive eXtended Reality training fueled by artificial intelligence. The Journal of Defense Modeling and Simulation: Applications, Methodology Technology 2022;19:195-218.
- Agha RA, Fowler AJ. The role and validity of surgical simulation. Int Surg 2015;100:350-7. [Crossref] [PubMed]
- Shaye DA. The history of nasal reconstruction. Curr Opin Otolaryngol Head Neck Surg 2021;29:259-64. [Crossref] [PubMed]
- Owen H. Early use of simulation in medical education. Simul Healthc 2012;7:102-16. [Crossref] [PubMed]
- Cooper JB, Taqueti VR. A brief history of the development of mannequin simulators for clinical education and training. Postgrad Med J 2008;84:563-70. [Crossref] [PubMed]
- Satava RM. Historical review of surgical simulation--a personal perspective. World J Surg 2008;32:141-8. [Crossref] [PubMed]
- Nam JG, Lee W, Jeong B, et al. Three-Dimensional Printing of Congenital Heart Disease Models for Cardiac Surgery Simulation: Evaluation of Surgical Skill Improvement among Inexperienced Cardiothoracic Surgeons. Korean J Radiol 2021;22:706-13. [Crossref] [PubMed]
- Yamada T, Osako M, Uchimuro T, et al. Three-Dimensional Printing of Life-Like Models for Simulation and Training of Minimally Invasive Cardiac Surgery. Innovations (Phila) 2017;12:459-65. [Crossref] [PubMed]
- Robinson DA, Piekut DT, Hasman L, et al. Cadaveric Simulation Training in Cardiothoracic Surgery: A Systematic Review. Anat Sci Educ 2020;13:413-25. [Crossref] [PubMed]
- Bedetti B, Bertolaccini L, Patrini D, et al. Virtual simulation and learning new skills in video-assisted thoracic surgery. Video-assist Thorac Surg 20025;3:35.
- Ujiie H, Chiba R, Yamaguchi A, et al. Developing a Virtual Reality Simulation System for Preoperative Planning of Robotic-Assisted Thoracic Surgery. J Clin Med 2024;13:611. [Crossref] [PubMed]
- Ujiie H, Yamaguchi A, Gregor A, et al. Developing a virtual reality simulation system for preoperative planning of thoracoscopic thoracic surgery. J Thorac Dis 2021;13:778-83. [Crossref] [PubMed]
- Alaker M, Wynn GR, Arulampalam T. Virtual reality training in laparoscopic surgery: A systematic review & meta-analysis. Int J Surg 2016;29:85-94. [Crossref] [PubMed]
- Seymour NE. VR to OR: a review of the evidence that virtual reality simulation improves operating room performance. World J Surg 2008;32:182-8. [Crossref] [PubMed]
- Tan SSY, Sarker SK. Simulation in surgery: a review. Scott Med J. 2011;56:104-9. [Crossref] [PubMed]
- Dadario NB, Quinoa T, Khatri D, et al. Examining the benefits of extended reality in neurosurgery: A systematic review. J Clin Neurosci 2021;94:41-53. [Crossref] [PubMed]
- Alexander C, Loeb AE, Fotouhi J, et al. Augmented Reality for Acetabular Component Placement in Direct Anterior Total Hip Arthroplasty. J Arthroplasty 2020;35:1636-1641.e3. [Crossref] [PubMed]
- Liu H, Wu J, Tang Y, et al. Percutaneous placement of lumbar pedicle screws via intraoperative CT image-based augmented reality-guided technology. J Neurosurg Spine 2019;32:542-7. [Crossref] [PubMed]
- Botden SM, Buzink SN, Schijven MP, et al. Augmented versus virtual reality laparoscopic simulation: what is the difference? A comparison of the ProMIS augmented reality laparoscopic simulator versus LapSim virtual reality laparoscopic simulator. World J Surg 2007;31:764-72. [Crossref] [PubMed]
- Lohre R, Bois AJ, Pollock JW, et al. Effectiveness of Immersive Virtual Reality on Orthopedic Surgical Skills and Knowledge Acquisition Among Senior Surgical Residents: A Randomized Clinical Trial. JAMA Netw Open 2020;3:e2031217. [Crossref] [PubMed]
- Kockro RA, Killeen T, Ayyad A, et al. Aneurysm Surgery with Preoperative Three-Dimensional Planning in a Virtual Reality Environment: Technique and Outcome Analysis. World Neurosurg 2016;96:489-99. [Crossref] [PubMed]
- Yan EG, Rennert RC, Levy DM, et al. Three-Dimensional Modeling of Complex Pediatric Intracranial Aneurysmal Malformations With a Virtual Reality System. Simul Healthc 2021;16:295-300. [Crossref] [PubMed]
- Porpiglia F, Checcucci E, Amparore D, et al. Three-dimensional Augmented Reality Robot-assisted Partial Nephrectomy in Case of Complex Tumours (PADUA ≥10): A New Intraoperative Tool Overcoming the Ultrasound Guidance. Eur Urol 2020;78:229-38. [Crossref] [PubMed]
- George EI, Smith R, Levy JS, et al. Simulation in robotic surgery. In: Stefanidis D, Korndorffer JR, Sweet R, editors. Comprehensive Healthcare Simulation: Surgery and Surgical Subspecialties. Cham: Springer International Publishing; 2019:191-220.
- Williams TP, Klimberg V, Perez A. Tele-education assisted mentorship in surgery (TEAMS). J Surg Oncol 2021;124:250-4. [Crossref] [PubMed]
- Li C, Tong Y, Long Y, et al. Extended reality with HMD-assisted guidance and console 3D overlay for robotic surgery remote mentoring. IEEE Robot Autom Lett 2024;9:9135-42. [Crossref]
- Lee D, Bathish MA, Nelson J. Transforming Nursing Education: Developing Augmented Reality Procedural Training. Cyberpsychol Behav Soc Netw 2024;27:372-8. [Crossref] [PubMed]
- Seymour NE, Røtnes JS. Challenges to the development of complex virtual reality surgical simulations. Surg Endosc 2006;20:1774-7. [Crossref] [PubMed]
- Laspro M, Groysman L, Verzella AN, et al. The use of virtual reality in surgical training: implications for education, patient safety, and global health equity. Surgeries 2023;4:635-46. [Crossref]
- Luong T, Cheng YF, Mobus M, et al. Controllers or Bare Hands? A Controlled Evaluation of Input Techniques on Interaction Performance and Exertion in Virtual Reality. IEEE Trans Vis Comput Graph 2023; Epub ahead of print. [Crossref] [PubMed]
- Weese J, Groth A, Nickisch H, et al. Generating anatomical models of the heart and the aorta from medical images for personalized physiological simulations. Med Biol Eng Comput 2013;51:1209-19. [Crossref] [PubMed]
- Marsden AL. Simulation based planning of surgical interventions in pediatric cardiology. Phys Fluids (1994) 2013;25:101303.
- Jadhav S, Kannanda V, Kang B, et al. Soft robotic glove for kinesthetic haptic feedback in virtual reality environments. Electron Imaging 2017;29:19-24. [Crossref]
- Boutin J, Kamoonpuri J, Faieghi R, et al. Smart haptic gloves for virtual reality surgery simulation: a pilot study on external ventricular drain training. Front Robot AI 2024;10:1273631. [Crossref] [PubMed]
- Sanders AJ, Luursema JM, Warntjes P, et al. Validation of open-surgery VR trainer. Stud Health Technol Inform 2006;119:473-6. [PubMed]
- Suwelack S, Sander C, Schill J, et al. Towards open-source, low-cost haptics for surgery simulation. Stud Health Technol Inform 2014;196:401-3. [Crossref] [PubMed]
- Kroft J, Ordon M, Po L, et al. Can Surgical “Warm-Up” With Instructor Feedback Improve Operative Performance of Surgical Trainees? J Minim Invasive Gynecol 2015;22:S17-8. [Crossref] [PubMed]
- Chugh AJ, Pace JR, Singer J, et al. Use of a surgical rehearsal platform and improvement in aneurysm clipping measures: results of a prospective, randomized trial. J Neurosurg 2017;126:838-44. [Crossref] [PubMed]
- Dhar E, Upadhyay U, Huang Y, et al. A scoping review to assess the effects of virtual reality in medical education and clinical care. Digit Health 2023;9:20552076231158022. [Crossref] [PubMed]
- Yilmaz R, Bakhaidar M, Alsayegh A, et al. Real-Time multifaceted artificial intelligence vs In-Person instruction in teaching surgical technical skills: a randomized controlled trial. Sci Rep 2024;14:15130. [Crossref] [PubMed]
- Bowen K, Barry M, Jowell A, et al. Virtual Exchange in Global Health: an innovative educational approach to foster socially responsible overseas collaboration. Int J Educ Technol High Educ 2021;18:32. [Crossref] [PubMed]
Cite this article as: Bui J, Lee D, Murthi S, Kantor T, Stegink C, Reddy RM. The role of extended reality in enhancing surgical training: a narrative review. Curr Chall Thorac Surg 2025;7:10.



